Ecosyste.ms: Awesome
An open API service indexing awesome lists of open source software.
https://github.com/moindalvs/a_guide_for_actuarial_science
What is Actuarial analyst ? what are their responsibilities, skills required and interview questions
https://github.com/moindalvs/a_guide_for_actuarial_science
Last synced: about 11 hours ago
JSON representation
What is Actuarial analyst ? what are their responsibilities, skills required and interview questions
- Host: GitHub
- URL: https://github.com/moindalvs/a_guide_for_actuarial_science
- Owner: MoinDalvs
- Created: 2022-11-03T14:06:41.000Z (about 2 years ago)
- Default Branch: main
- Last Pushed: 2023-02-24T13:46:01.000Z (over 1 year ago)
- Last Synced: 2023-03-08T12:08:12.812Z (over 1 year ago)
- Size: 539 KB
- Stars: 3
- Watchers: 1
- Forks: 0
- Open Issues: 0
-
Metadata Files:
- Readme: README.md
Awesome Lists containing this project
README
## 0.1 Table of Contents
1. [Actuarial Analyst](#1)
- 1.1 [Why work as an analyst?](#1.1)
- 1.2 [What does an Actuarial analysts do?](#1.2)
- 1.3 [How do I become an actuarial analyst?](#1.3)
- 1.4 [Job Responsibilities are the Main Difference](#1.4)
- 1.5 [Is the actuarial analyst career right for you?](#1.5)
- 1.6 [12 Types Of Actuaries And Their Role Description](#1.6)
2. [Actuarial science](#2)
3. [What is Risk?](#3)
- 3.1 [Types of Risks](#3.1)
- 3.2 [What Is Financial Risk?](#3.2)
4. [What is Insurance?](#4)
- 4.1 [Principles of Insurance](#4.1)
- 4.2 [Average Deviation](#4.2)
- 4.3 [What Is Liability Insurance?](#4.3)
- 4.4 [Characteristics of an Ideally Insurable Risk](#4.4)
5. [What Is the Morbidity Rate?](#5)
6. [What Is the Law of Large Numbers?](#6)
7. [Insurance obligation](#7)
8. [What Is Reinsurance?](#8)
- 8.1 [How Reinsurance Works](#8.1)
9. [Deductibles](#9)
10. [What Is Coinsurance?](#10)
11. [What Are Copays?](#11)
12. [Coinsurance vs. Copay: What's the Difference?](#12)
13. [Co-pay vs. Deductible: What’s the Difference?](#13)
14. [What Are Out-of-Pocket Maximums?](#14)
15. [What’s a High-Deductible Health Plan?](#15)
16. [In-Network vs. Out-of-Network](#16)
17. [In-Patient vs Out-Patient](#17)
18. [Stop-Loss Insurance 101](#18)
- 18.1 [There are two types of self-funded insurance:](#18.1)
19. [What is lasering?](#19)
20. [Definition of Technical Provisions](#20)
21. [Health Reimbursement Arrangement (HRA)?](#21)
22. [Health Savings Account (HSA)](#22)
23. [Prefered Provider Organization (PPO)](#23)
24. [Health Maintenance Organization (HMO)](#24)
25. [Point-of-Service (POS)](#25)
26. [What Is Incurred But Not Reported (IBNR)?](#26)
27. [Wholesale and Retail Insurance?](#27)
28. [Actuarial Common Interview Questions](#28)
# 1.) Actuarial Analyst
**Actuarial analysts provide pivotal financial information to financial institutions, insurance companies, and other businesses. They predominantly analyze data using statistical modeling and complex mathematical formulas to assess risk. Actuarial analysts report to credentialed actuaries.**
**Actuarial science is a deeply sought-after field that plays a high role in the success of a company. Actuarial analysts help accredited actuaries make strategic decisions and communicate solutions for deeply complex financial issues.**
**Many types of companies find value in hiring actuarial analysts. Some of the most common employers of actuarial analysts are insurance companies, consulting firms, government, hospitals, banks, and investment firms. There is typically a divide between those in life disciplines (life and health insurance) and those in non-life disciplines (auto, home, and property insurance).**
**The day-to-day role of an actuarial analyst involves quite a bit of mathematical work and analysis. It’s a fairly competitive field, meaning that commitment and strong collegiate performance can give you a leg up when searching for a job.**
## If you’re looking for a professional career that involves solving problems, working with tons of numbers, and analysing data, well, then becoming an actuarial analyst may just be the job for you!
### Learn about the key requirements, duties, responsibilities, and skills that should be in an actuarial analyst job description.
### What is an actuarial analyst?
Before we talk about what an actuarial analyst is, it’s important that you first understand what an actuary is. Because, an actuarial analyst is just the job title of someone that is working in a role as an actuary, but isn’t yet a fully qualified actuary.
#### Actuary Job Details
An actuary is someone that quantifies risk. They use statistics, probabilities, and financial concepts in order put a financial dollar value on an event that may or may not occur in the future.
They typically work in insurance companies determining how much to charge for insurance policies, or figuring out how much money an insurance company needs to save in order to keep their commitments to policyholders.
The key thing to understand here is that becoming a fully qualified actuary takes many years. Usually between 7-10 years actually. But anyone that is in the process of becoming an actuary can still work in the actuarial field (as an actuarial analyst) before they’re fully qualified.
#### 1.1 ) Why work as an analyst?
This allows them to gain valuable work experience and industry knowledge well before they’re fully qualified. That’s important because fully qualified actuaries have a huge amount of responsibility and their job requires lots of professional judgement that can only be attained through years of experience.
So, sometimes the job title of an actuary that isn’t yet fully qualified is “actuarial analyst”. But this is just a job title. Another common job title (which means the exact same thing) is “actuarial associate”.
In some cases, the job title may just be “actuary”, “pricing actuary”, “valuation actuary” or something else along those lines. The job titles often vary from company to company.
#### 1.2 ) What does an Actuarial analysts do?
Actuarial analysts use statistical models to analyze data and assess risk. Many industries employ actuarial analysts, but the insurance industry particularly uses their knowledge and skills to design and price insurance policies.
It’s most common for an actuarial analyst to be heavily involved in either the calculation of insurance premiums or reserves. Reserves are the industry term for the amount of assets (bonds, stocks, mortgages, private placements, etc.) that an insurance company needs to own in order to ensure that they are financially stable.
Since insurance contracts can last 50+ years, it’s important that insurance companies properly manage their cash flows to ensure they have enough money to pay any insurance claims that are made in the future. That’s why reserves are so important.
An actuarial analyst isn’t a fully qualified actuary and is still gaining knowledge and expertise in their industry. Because of this, they often do much of the technical work required in order for their immediate manager (usually a fully qualified actuary) and upper management to make informed decisions.
By doing much of the technical work, an actuarial analyst is able to dig deep into the details and fully understand how actuarial processes work, how reported values are calculated, and they’ll often investigate inconsistencies in data.
Having this in-depth insight into the business workings allows the actuarial analyst to develop in their career and become prepared for the requirements of a fully-qualified actuary.
#### 1.3 ) How do I become an actuarial analyst?
There are two primary requirements that are necessary in order to be an actuarial analyst. First, you need to get a Bachelor’s degree, and second you need to pass at least 1 actuarial exam.
### Bachelor’s Degree
Due to the nature of an actuarial analyst position, you need to be well-versed in topics such as finance, business, statistics and economics.
As a result, the first thing you’d need to do in order to become one is get a Bachelor’s degree. It doesn’t have to be a degree in one of the fields listed above, but it would be helpful in your career if it was. Actually, a degree technically isn’t required, but nearly all good candidates have one and an actuarial employer would be unlikely to hire someone without one.
Another option is to get your Bachelor’s degree in “actuarial science”. These courses are only offered in certain colleges and universities. They teach math concepts that are very specific to the actuarial field.
## 1.4 ) Job Responsibilities are the Main Difference
Aside from those requirements and the salary, there is a big difference in the job responsibilities of an actuarial analyst and a fully qualified actuary.
### The Actuary
A fully-qualified actuary will often be using their knowledge and expertise in order to make critical business decisions. They’ll rely extensively on their past experiences in the industry, as well as concepts learned by studying for the later actuarial exams.
They’ll often use data summaries, industry reports, and company objectives in order to make decisions that are best for the company overall. To do this, an actuary will regularly collaborate with other actuaries in the company in order to get different perspectives, discover potential drawbacks and ideas.
Combining expertise in this way can be very powerful and reduces the possibility of overlooking potential issues that may arise in the future.
### The Actuarial Analyst
On the other hand, an actuarial analyst often isn’t involved in as many of these high-level, decision-making collaborations. Instead, the analyst is typically responsible for collecting, analysing and summarizing all the data that is needed for the fully-qualified actuaries to make their decisions.
The actuaries need to take into consideration many different factors when making decisions, and quite often it requires large amounts of data to be summarized into numbers that can easily be interpreted. This is where the analyst comes in.
The analyst will put everything together for the actuaries that they report to. This gives the actuaries more time for higher-level thinking and decision making rather than being caught up in the weeds of all the data.
Analysts are often also responsible for the monthly, quarterly, and annual reporting processes that need to be completed by the actuarial departments. These are often fairly manual processes that require the analyst to fully understand the data, calculations and results.
Although analysts may not attend all the collaboration meetings, their inputs and perspectives are still very valuable. Oftentimes the actuary that they’re providing data to doesn’t know all the nuances of the data, calculations and results that are produced.
So, an analyst can make them aware of any potential problems that may arise in the actual implementation of business changes and decisions.
As may be expected, the job responsibilities of an actuarial analyst are much more technical than those of an actuary. But both are needed in order to allow the insurance company to function.
### Actuarial Analyst vs Actuarial Assistant. Are they the same?
An actuarial analyst and an actuarial assistant are not the same job. An actuarial analyst does most of the technical work involving gathering, analysing, and interpreting data whereas an actuarial assistant often works alongside a team of actuarial analysts. The assistant will help do the tasks that need to be done but don’t require the expertise and skill set of the analysts.
In order to do their job, and actuarial analyst often needs to know how to write code to automate tasks. They also spend time formatting reports, cleaning data, and entering data into the computer.
But, these tasks aren’t really utilizing the specialized knowledge and analytical abilities of the analyst. So, it makes sense to have someone else do these tasks rather than the analyst. The analyst can then spend more time on understanding and interpreting results.
Having an actuarial assistant also makes sense from a financial standpoint because they don’t need to be paid as high of a salary as an actuarial analyst would.
Having actuarial assistants is a company choice. Some companies have them, and others don’t. But for someone looking to get into an actuarial analyst position, an actuarial assistant job can be very beneficial in making connections and learning about actuarial work.
## 1.5 ) Is the actuarial analyst career right for you?
Most people don’t go into the actuarial profession without the intention to become a fully qualified actuary. The actuarial analyst job is a stepping stone on that journey. So, really, you have to think about whether a career as an actuary is right for you.
If you decide to stop pursuing a career as an actuary and stay as an actuarial analyst, you’ll be limited in your career growth opportunities and it may be difficult to switch companies (to another actuarial analyst position). Your exam process and work ethic will play a big part in whether this is possible.
#### You need to be goal oriented and persistent.
Getting through all the actuarial exams can be quite a long and difficult process. You need to be able to persevere through failures, and enjoy the challenge that each exam brings.
If you’re goal oriented, you’ll strive to complete the exams quickly, and the reward of a raise will motivate you.
#### Love problem solving.
Actuarial work regularly involves figuring out solutions to problems and a lot of judgement. Typically there’s no right or wrong answer in this field so it’s an analyst’s job to determine creative solutions and assess the advantages and disadvantages of each.
#### Enjoy math and working with numbers (a lot).
Actuaries work with numbers every single day. Most of them love to dig into the details and figure out why trends are occurring. Actuaries use numbers and mathematical concepts in order to make business decisions that are in the best interest of the company and its policyholders.
**`If you’re not good at math or don’t enjoy it, a career as an actuary likely won’t interest you for very long.`**
### Skills an actuarial analyst needs
Not everyone is cut out for the life of an actuarial analyst; it takes a very special set of skills. Thankfully, many of these skills are not inherent and can be developed through determination and hard work. These necessary skills are:
+ Specialized math knowledge in calculus, statistics, and probability
+ Analytical, project management, and problem solving skills
+ Finance, accounting, economics
+ Interpersonal communication
Computer skills such as simple coding, formulating spreadsheets, running statistical analysis programs, database manipulation, and programming languages
An actuarial analyst must be self-motivated, creative, both independent and collaborative at times, and have a strong sense of ambition. Having an understanding for the common industries that actuarial analysts are employed in such as insurance, banking, and government can also set you ahead as a candidate in the field.
## Actuarial Analyst Job Description Template
We are looking for a dedicated actuarial analyst with a strong statistics background to join our team. You will be using statistical modeling to analyze data relating to mortality, accidents, retirement, finance, etc. Other responsibilities include reporting to actuaries, providing technical support, and verifying the validity of data sources.
Successful candidates will be those who demonstrate exceptional critical thinking, possess a working knowledge of statistical analysis software, and can communicate complex statistical findings in an easy-to-understand way.
### **Actuarial Analyst Responsibilities:**
+ **Using advanced statistics and modeling to understand data.**
+ **Assisting actuaries with technical support and analysis.**
+ **Producing reports on analysis findings.**
+ **Identifying liabilities and risks.**
+ **Identifying trends.**
+ **Helping to design and price insurance policies.**
+ **Verifying data sources.**
+ **Identifying new sources of data.**
+ **Developing processes for improved data analysis and reporting.**
### **Actuarial Analyst Requirements:**
+ **Bachelor's degree in mathematics, statistics, or actuarial science.**
+ **Exceptional mathematical and statistical knowledge and understanding.**
+ **Experience with spreadsheets and databases.**
+ **Working knowledge of statistical analysis programs such as Insightful S-PLUS and Wolfram Research Mathematica.**
+ **Excellent critical thinking, problem-solving, and communication skills**
+ **General understanding of computers and electronics**
+ **Basic knowledge of laws, legal codes, regulations, etc.**
+ **Basic understanding of business and finance.**
## 1.6 ) 12 Types Of Actuaries And Their Role Description
Actuarial science is a field of mathematics which studies and quantifies financial risk using probability and statistics. Students of actuarial science analyze financial implications of future events using mathematical and statistical methods.
Insurance companies, pension providers and various financial firms employ different types of actuaries to analyze their risks and liabilities, improve their financial decision making and evaluate the impact of financial and economic events.
Many colleges and universities offer a graduate degree in actuarial science which consists of several interrelated subjects like mathematics, statistics, economics, finance, probability theory and computer science.
Getting a degree in actuarial science is challenging. You need to pass a series of actuarial exams that will make you a certified actuary. It requires that you have fairly good technical, mathematical and analytical skills.
### There are many different types of actuaries employed across various industries with insurance sector being the top recruiter. Let’s have a look at who they are and what they do.
+ **Life Insurance Actuary**
+ **Health Insurance Actuary**
+ **Pension Actuary**
+ **Property And Casualty Actuary**
+ **Enterprise Risk Management Actuary**
+ **Investment Actuary**
+ **Finance Actuary**
+ **Pricing Actuary**
+ **Valuation Actuary**
+ **Reinsurance Pricing Actuary**
+ **Corporate Actuary**
+ **Forensic Actuary**
### Life Insurance Actuary
Among all the actuaries, life insurance actuary is one of the most common. These types of actuaries work for insurance and reinsurance companies which offer products like whole life insurance and term life insurance.
Insurance companies sell thousands of policies every year. Life insurance actuaries help these companies to properly price the life insurance policy and determine the insurance premium for such policies.
Life insurance actuaries use mortality rates to find out the percentage of people that will die in any given year. The mortality rate for any person depends on various factors like age, gender and smoking status.
They use these mortality rates to find out what should be the insurance premium for different policies. Someone who is expected to live more than 30 years will pay lower premium than someone who is expected to live less than 10 years.
Life insurance claims are very hard to predict accurately as these are high cost low frequency claims. There is lot of variability involved in the amount insurance company has to pay each year.
Life insurance actuaries also have to take into account the lapse rate which is the rate at which the policyholders cancel their policies. High frequency of early cancellations can result in high insurance premiums because most of the expenses are incurred at the beginning of the policy.
### Health Insurance Actuary
Health insurance actuaries work with health insurance companies and help them to predict the actual cost of healthcare covered under insurance contract. These predictions are based on various factors like family history, occupation and geographical location.
Mostly health insurance actuaries are involved in designing group insurance plans which cover employer disability, dental, health and medication. They also provide policies to people who are self employed or employees who are not covered by their employer.
Actuaries that work in disability insurance try to predict how many policyholders will be unable to work each year and how much money insurance company will have to pay these policyholders to replace their lost income.
These types of actuaries also have to determine how soon the policy holder can get back to work because the longer the policyholder is out of work the longer the insurance company have to pay them.
Health insurance claims are fairly easy to predict accurately as these are considered as low cost high frequency claims. Health insurance actuaries use past data in order to predict how much money the policyholders will be spending on prescription drugs, dental benefits and health related sessions.
These types of actuaries use lot of data for analysis and most of the data is collected from policyholders. They also have to take into account the demographics, lapse rates, claim frequency and increasing medication costs.
### Pension Actuary
Pension actuaries are responsible for calculating the employer’s contribution as well as retirement benefits of pension plan participants. These types of actuaries help the plan sponsors to calculate sufficient balance required to fund the retirement benefits of pension plan participants.
These calculations are based on various assumptions about future events like retirement, disability, death and termination of employment. They also take into account the future economic events like interest rates and increase in salaries.
Pension actuaries do not deal with any insurance product but they create and price investment and annuity products which help the individuals to be financially prepared after retirement. These types of actuaries work with employers to develop retirement pension plans for employees.
Pension actuaries use current interest rates to determine the pricing of annuities. If interest rates rise, then the price of annuity will decrease as the insurance company will be able to earn more form increasing interest rates.
Pension actuaries try to predict how long people will live and how long people will be receiving payments. They also use mortality rates to determine the price of an annuity. Since mortality rates are higher among older people, pension actuaries would expect fewer annuity payments, hence reducing the price of the annuity.
### Property And Casualty Actuary
Property and casualty actuaries are one of the most common types of general actuaries or non-life actuaries. They work with general insurance companies and help them develop insurance policies that ensure against property loss and liabilities resulting from accidents, natural disasters or any other events.
These types of actuaries use their skills to analyze the risk emerging from climate change, ride sharing, automated vehicles and cyber liability. They are also responsible for pricing, predictive modeling, capital and risk management, strategic and financial management and catastrophe modeling.
Claims under property and casualty insurance are considered as high frequency low severity claims. These types of claims are easy to predict accurately. Vehicle insurance actuaries predict the probability of the policyholder getting into an accident and also the cost of the accident.
Property insurance actuaries determine the likelihood of property getting damaged from flooding, fire, extreme weather and anything else that can cause damage to the property. Such policy also covers for the loss due to theft of the items within the house.
Similar to health insurance actuaries, these types of actuaries also collect most of their data from policyholders. Demographics play an important role and due to high frequency of claims there is lot of data available for analysis.
Companies that provide property and casualty insurance in high crime areas will demand a higher premium for their insurance policies compared to the companies which insures people in low crime areas.
### Enterprise Risk Management Actuary
Enterprise risk management is a process of identifying critical risks faced by an organization, prioritizing them, quantifying their financial impact and developing organizational solutions to address them.
Primary responsibility of an enterprise risk management actuary is to consolidate all the risks which are faced by the company and determine the financial impact due to those risks. Their skills are not just limited to insurance companies.
One of the examples of an ERM actuary is to determine the cost and the potential impact of negative reputation on the organization. Any negative reputation would result in lower sales, lower revenue and legal charges.
Depending upon the severity, loss of reputation can even force the company to go out of business. The ERM actuary recognizes this and encourages the company to keep enough capital to survive such situations.
This is very important for insurance companies as thousands of people rely on them to collect insurance claims when the time comes. Enterprise risk management can prevent such companies from going out of business and protect their policyholders.
### Investment Actuary
Investment actuary is an actuary that either manages investments directly or provides an advice on how to manage investments. As with all the actuaries, their main focus tends to be on risk management.
Investment actuaries work in areas like investment banking, investment consulting, investment management and retail financial advice. They are also involved in day to day activities in capital markets, derivative markets, forex and property markets.
Investment actuaries have strong analytical skills and deep understanding about interaction between assets and liabilities which is very important while advising or managing assets backing insurance and pension liabilities.
### Finance Actuary
Finance actuaries work in areas like corporate finance, mergers and acquisitions, capital management and financial reporting. They have strong understanding about the working of insurance companies and other financial institutions.
Finance actuaries and financial analysts have very similar responsibilities as they both are involved in analyzing the data and reducing the risk of financial troubles. However, finance actuaries work closely with insurance companies whereas financial analysts are more focused on investment strategies.
The job responsibility of a finance actuary includes gathering data, performing calculations, evaluating investment options, determining the likelihood of any specific event occurring and recommending policies or investments to other people.
### Pricing Actuary
Pricing actuaries are statisticians who primarily work for financial industries or insurance companies. They use their analytical and math skills to determine the price of the products by analyzing data and calculating risks.
These types of actuaries collect and analyze statistical data to determine the claim payout in event of death, serious injury, property loss, disability or claims resulting from any casualties. They use this data to develop profitable yet competitive product pricing.
The decisions made by pricing actuaries should be high enough to cover the expenses and cost associated with insurance claims and to maximize the returns for insurance company. They are also involved in developing the policies and plans for new products and designing financially sound insurance and pension plans.
### Valuation Actuary
Valuation actuaries are responsible for calculating the reserves for life insurance and annuity companies, calculating the liabilities for financial statements and determining the valuation of the companies involved in mergers and acquisitions.
They ensure that the insurance company has enough reserves to pay for the expenses and claims that will be due in future. Once reserves are calculated they are also responsible for creating the source of earnings.
These types of actuaries use different valuation models to determine the reserves required by insurance company. In order to keep these valuation models up to date and accurate, they have to update the assumptions used in these models on an annual basis.
### Reinsurance Pricing Actuary
Like primary insurance, reinsurance is also a mechanism to spread out the risk. The reinsurer takes on some portion of the risk assumed by the primary insurer and charges an appropriate premium for that.
The main difference between reinsurance and primary insurance is that reinsurance contracts are more favorable to the buyer. The reinsurance pricing actuaries are responsible for estimating the risk and calculating the pricing of reinsurance contracts.
### Corporate Actuary
Corporate actuary is mostly involved either with product development or with financial reporting and valuation. They have special financial knowledge to analyze the results, feedback and the product pricing process.
Corporate actuaries also involved in corporate mergers and acquisitions, expense management, risk management, capital management, asset liability management and also in developing new performance measures for the company.
### Forensic Actuary
Forensic actuaries have a key role to play in providing litigation support in insurance and reinsurance cases. They serve as an expert witness where loss reserves and pricing issues are important. They can also act as arbitrators while resolving a dispute for insurance policy or reinsurance contract.
[Table of Content](#0.1)
___
# 2.) Actuarial science
It is a field of mathematics which studies and quantifies financial risk using probability and statistics. Students of actuarial science analyze financial implications of future events using mathematical and statistical methods.
Insurance companies, pension providers and various financial firms employ different types of actuaries to analyze their risks and liabilities, improve their financial decision making and evaluate the impact of financial and economic events.
Many colleges and universities offer a graduate degree in actuarial science which consists of several interrelated subjects like mathematics, statistics, economics, finance, probability theory and computer science.
Getting a degree in actuarial science is challenging. You need to pass a series of actuarial exams that will make you a certified actuary. It requires that you have fairly good technical, mathematical and analytical skills.
[Table of Content](#0.1)
___
# 3.) What is Risk?
Risk is an possibility of an adverse deviation from a desired outcome with uncertainty of expected or hoped for. Risk is the chance or probability that a person will be harmed or experience an adverse health effect if exposed to a hazard. It may also apply to situations with property or equipment loss, or harmful effects on the environment.
Risk probability, or likelihood, is the possibility of a risk event occurring. The likelihood can be expressed in both a qualitative and quantitative manner. When discussing probability in a qualitative manner, terms such as frequent, possible, rare etc. are used
#### Explanation
Risk Insurance shall involve assessing the price to be paid to Insurance policyholders who have suffered from the loss that occurred to them, which is covered by the policy. It involves various types of risks such as theft, loss, or damage of property or also may involve someone being injured; there is a chance that something unexpected or harmful may happen at any point in time.
It evolves in calculating the pay of the financial value for the damages that might occur to the insured property or item that might be lost, injured, or destroyed accidentally or often occur to happen. It also states how much it would cost to replace
or repair such an insured item to cover the loss suffered by the policyholder in case of such damage. Insurers shall calculate claims and evaluate their risks.
## 3.1) Types of Risks
The following are the different types of risk in insurance:

#### 1 – Pure Risk
Pure risk refers to the situation where it is certain that the outcome will lead to loss of the person only or maximum it could lead to the condition of the no loss to the person, but it can never cause profit to the person. An example of pure risk includes the possibility of damage to the house due to natural calamity.
In case any natural calamity occurs, it will damage the house of the person and its household items, or it will not affect the person’s home and household items. Still, this natural calamity will not give any profit or gain to the person. So, this will fall under the pure risk, and these risks are insurable.
#### 2 – Speculative Risk
Speculative risk refers to the situation where the direction of the outcome is not specific, i.e., it could lead to a condition of loss, profit, or no-loss. These risks are generally not insurable. An example of speculative risk includes the purchase of the shares of a company by a person.
Now, the prices of the shares can go in any direction, and a person can make either loss, profit, or no loss, no profit at the time of the sale of those shares. So, this will fall under the Speculative risk.
#### 3 – Financial Risk
Financial risk refers to the danger in which the outcome of the event is measurable in terms of the money, i.e., any loss that could occur due to the risk can be measured by the concerned person in monetary value. An example of financial risk includes a loss to the goods in the warehouse of the company due to the fire. These risks are insurable and are generally the main subjects of the insurance.
#### 4 – Non-Financial Risk
Non-Financial risk refers to the risk in which the outcome of the event is not measurable in terms of the money, i.e., any loss that could occur due to the risk cannot be measured by the concerned person in the monetary value. An example of the non-financial risk includes the risk of poor selection of the brand while purchasing mobile phones. These risks are uninsurable since they cannot be measured.
#### 5 – Particular Risk
Particular risk refers to the risk which arises mainly because of the actions or the interventions of the individual or the group of some individuals. So, the origin of the particular risk by individual-level and impact of the same is felt at a localized level. An example of a specific chance includes an accident on the bus. These risks are insurable and are generally the main subjects of the insurance.
#### 6 – Fundamental Risk
Fundamental risk refers to the risk which arises due to the causes which are not under the control of any person. So, it can be said that the fundamental risk is impersonal in its origin and the consequences. The impact of these risks is essentially on the group, i.e., it affects the large population. The fundamental risk includes risks on the group by events such as natural calamity, economic slowdown, etc. These risks are insurable.
##### Fundamental risk vs. particular risk
Fundamental risk is risk that affects entire societies or a large population within a society. Natural disasters, such as earthquakes and hurricanes, fall into the category of fundamental risk, as do phenomena such as inflation and war, which typically affect large numbers of people. In distinction to static risk, fundamental risk may or may not be insurable.
Particular risk, in contrast to fundamental risk, refers to risks that affect an individual, such as a fire that destroys a family home, theft of a car or robbery. Particular risk can be insured.
#### 7 – Static Risk
Static risk refers to the risk which remains constant over the period and is generally not affected by the business environment. These risks arise from human mistakes or actions of nature. An example of static risk includes the embezzlement of funds in a company by its employees. They are generally easily insurable as they are easy to measure.
#### 8 – Dynamic Risk
Dynamic risk refers to the risk which arises when there are any changes in the economy. These risks are generally not easy to predict. These changes might bring financial losses to the members of the economy. An example of the dynamic risk includes the changes in the income of the persons in an economy, their tastes, preferences, etc. They are generally not easily insurable.
##### Static risk vs. dynamic risk
Static risk is a type of pure risk that is predictable, measurable and doesn't change. It is a type of pure risk because it is not chosen and no financial gain can come from static risk.
Insuranceopedia, an online repository of financial information and insurance definitions, defines static risk as "risks that involve losses brought about by acts of nature or by malicious and criminal acts by another person. These losses refer to damage or loss to property or entity that is not caused by the economy." A flood is an example of static risk. According to Insuranceopedia, static risks "are more easily taken care of by insurance coverage because of their relative predictability."
Dynamic risk, in contrast to static risk, is a "risk brought on by sudden and unpredictable changes in the economy," according to Insuranceopedia. This type of risk is difficult to measure, sometimes resulting in sizable losses for individuals and businesses. Insuranceopedia pointed to the COVID-19 pandemic as an example of dynamic risk, not only due its unpredictability, but also its impact on many lines of insurance coverage, including business interruption, trade credit and cyber liability insurance. A recession is another example of a dynamic risk, as well as a fundamental risk.
### 3.2) What Is Financial Risk?
Financial risk is the possibility of losing money in a business venture or investment. There are several types of financial risks, such as credit risk, liquidity risk, and operational risk. A financial risk is a potential loss of capital to an interested party.
In other words, financial risk is a danger that can translate into the loss of capital. It relates to the odds of money loss.
In case of a financial risk, there is a possibility that a company’s cash flow might prove insufficient to satisfy its obligations. Some common financial risks are credit, operational, foreign investment, legal, equity, and liquidity risks.
In government sectors, financial risk implies the inability to control monetary policy and or other debt issues. Learn more about how financial risk is associated with different sectors, be it business, government, market, or individuals.
#### Types of Financial Risks
Risk can be referred to like the chances of having an unexpected or negative outcome. Any action or activity that leads to loss of any type can be termed as risk. There are different types of risks that a firm might face and needs to overcome. Widely, risks can be classified into three types: Business Risk, Non-Business Risk, and Financial Risk.
+ **Business Risk:** These types of risks are taken by business enterprises themselves in order to maximize shareholder value and profits. As for example, companies undertake high-cost risks in marketing to launch a new product in order to gain higher sales.
+ **Non- Business Risk:** These types of risks are not under the control of firms. Risks that arise out of political and economic imbalances can be termed as non-business risk.
+ **Financial Risk:** Financial Risk as the term suggests is the risk that involves financial loss to firms. Financial risk generally arises due to instability and losses in the financial market caused by movements in stock prices, currencies, interest rates and more.
### Types of Financial Risks
Risk Types: The different types of risks are categorized in several different ways. Risks are classified into some categories, including market risk, credit risk, operational risk, strategic risk, liquidity risk, and event risk.
Financial risk is one of the high-priority risk types for every business. Financial risk is caused due to market movements and market movements can include a host of factors. Based on this, financial risk can be classified into various types such as Market Risk, Credit Risk, Liquidity Risk, Operational Risk, and Legal Risk.

#### Market Risk:
This type of risk arises due to the movement in prices of financial instrument. Market risk can be classified as Directional Risk and Non-Directional Risk. Directional risk is caused due to movement in stock price, interest rates and more. Non-Directional risk, on the other hand, can be volatility risks.
#### Credit Risk:
This type of risk arises when one fails to fulfill their obligations towards their counterparties. Credit risk can be classified into Sovereign Risk and Settlement Risk. Sovereign risk usually arises due to difficult foreign exchange policies. Settlement risk, on the other hand, arises when one party makes the payment while the other party fails to fulfill the obligations.
#### Liquidity Risk:
This type of risk arises out of an inability to execute transactions. Liquidity risk can be classified into Asset Liquidity Risk and Funding Liquidity Risk. Asset Liquidity risk arises either due to insufficient buyers or insufficient sellers against sell orders and buys orders respectively.
#### Operational Risk:
This type of risk arises out of operational failures such as mismanagement or technical failures. Operational risk can be classified into Fraud Risk and Model Risk. Fraud risk arises due to the lack of controls and Model risk arises due to incorrect model application.
#### Legal Risk:
This type of financial risk arises out of legal constraints such as lawsuits. Whenever a company needs to face financial losses out of legal proceedings, it is a legal risk.
[Table of Content](#0.1)
___
# 4.) What is Insurance?
Represented in a form of policy, Insurance is a contract in which the individual or an entity gets the financial protection, in other words, reimbursement from the insurance company for the damage (big or small) caused to their property.
The insurer and the insured enter a legal contract for the insurance called the insurance policy that provides financial security from the future uncertainties.
In simple words, insurance is a contract, a legal agreement between two parties, i.e., the individual named insured and the insurance company called insurer. In this agreement, the insurer promises to help with the losses of the insured on the happening contingency. The insured, on the other hand, pays a premium in return for the promise made by the insurer.
The contract of insurance between an insurer and insured is based on certain principles, let us know the principles of insurance in detail.
#### What’s a Health Insurance Premium?
A health insurance premium is the upfront cost of maintaining health insurance coverage. Most premiums are paid on a monthly or biweekly basis. If your healthcare is provided by your employer, they will usually deduct the premium from your paycheck.
## 4.1 ) Principles of Insurance
The concept of insurance is risk distribution among a group of people. Hence, cooperation becomes the basic principle of insurance.
To ensure the proper functioning of an insurance contract, the insurer and the insured have to uphold the 7 principles of Insurances mentioned below:
+ Utmost Good Faith
+ Proximate Cause
+ Insurable Interest
+ Indemnity
+ Subrogation
+ Contribution
+ Loss Minimization
Let us understand each principle of insurance with an example.
#### Principle of Utmost Good Faith
The fundamental principle is that both the parties in an insurance contract should act in good faith towards each other, i.e. they must provide clear and concise information related to the terms and conditions of the contract.
The Insured should provide all the information related to the subject matter, and the insurer must give precise details regarding the contract.
Example – Jacob took a health insurance policy. At the time of taking insurance, he was a smoker and failed to disclose this fact. Later, he got cancer. In such a situation, the Insurance company will not be liable to bear the financial burden as Jacob concealed important facts.
#### Principle of Proximate Cause
This is also called the principle of ‘Causa Proxima’ or the nearest cause. This principle applies when the loss is the result of two or more causes. The insurance company will find the nearest cause of loss to the property. If the proximate cause is the one in which the property is insured, then the company must pay compensation. If it is not a cause the property is insured against, then no payment will be made by the insured.
Example –
+ **Due to fire, a wall of a building was damaged, and the municipal authority ordered it to be demolished. While demolition the adjoining building was damaged. The owner of the adjoining building claimed the loss under the fire policy. The court held that fire is the nearest cause of loss to the adjoining building, and the claim is payable as the falling of the wall is an inevitable result of the fire.**
+ **In the same example, the wall of the building damaged due to fire, fell down due to storm before it could be repaired and damaged an adjoining building. The owner of the adjoining building claimed the loss under the fire policy. In this case, the fire was a remote cause, and the storm was the proximate cause; hence the claim is not payable under the fire policy.**
#### Principle of Insurable interest
This principle says that the individual (insured) must have an insurable interest in the subject matter. Insurable interest means that the subject matter for which the individual enters the insurance contract must provide some financial gain to the insured and also lead to a financial loss if there is any damage, destruction or loss.
Example – the owner of a vegetable cart has an insurable interest in the cart because he is earning money from it. However, if he sells the cart, he will no longer have an insurable interest in it.
To claim the amount of insurance, the insured must be the owner of the subject matter both at the time of entering the contract and at the time of the accident.
#### Principle of Indemnity
This principle says that insurance is done only for the coverage of the loss; hence insured should not make any profit from the insurance contract. In other words, the insured should be compensated the amount equal to the actual loss and not the amount exceeding the loss. The purpose of the indemnity principle is to set back the insured at the same financial position as he was before the loss occurred. Principle of indemnity is observed strictly for property insurance and not applicable for the life insurance contract.
Example – The owner of a commercial building enters an insurance contract to recover the costs for any loss or damage in future. If the building sustains structural damages from fire, then the insurer will indemnify the owner for the costs to repair the building by way of reimbursing the owner for the exact amount spent on repair or by reconstructing the damaged areas using its own authorized contractors.
#### Principle of Subrogation
Subrogation means one party stands in for another. As per this principle, after the insured, i.e. the individual has been compensated for the incurred loss to him on the subject matter that was insured, the rights of the ownership of that property goes to the insurer, i.e. the company.
Subrogation gives the right to the insurance company to claim the amount of loss from the third-party responsible for the same.
Example – If Mr A gets injured in a road accident, due to reckless driving of a third party, the company with which Mr A took the accidental insurance will compensate the loss occurred to Mr A and will also sue the third party to recover the money paid as claim.
#### Principle of Contribution
Contribution principle applies when the insured takes more than one insurance policy for the same subject matter. It states the same thing as in the principle of indemnity, i.e. the insured cannot make a profit by claiming the loss of one subject matter from different policies or companies.
Example – A property worth Rs. 5 Lakhs is insured with Company A for Rs. 3 lakhs and with company B for Rs.1 lakhs. The owner in case of damage to the property for 3 lakhs can claim the full amount from Company A but then he cannot claim any amount from Company B. Now, Company A can claim the proportional amount reimbursed value from Company B.
#### Principle of Loss Minimisation
This principle says that as an owner, it is obligatory on the part of the insurer to take necessary steps to minimise the loss to the insured property. The principle does not allow the owner to be irresponsible or negligent just because the subject matter is insured.
Example – If a fire breaks out in your factory, you should take reasonable steps to put out the fire. You cannot just stand back and allow the fire to burn down the factory because you know that the insurance company will compensate for it.
#### Pure Risk vs. Speculative Risk
Insurance companies normally only indemnify against pure risks, otherwise known as event risks. A pure risk includes any uncertain situation where the opportunity for loss is present and the opportunity for financial gain is absent.
Speculative risks are those that might produce a profit or loss, namely business ventures or gambling transactions. Speculative risks lack the core elements of insurability and are almost never insured.
Examples of pure risks include natural events, such as fires or floods, or other accidents, such as an automobile crash or an athlete seriously injuring his or her knee. Most pure risks can be divided into three categories: personal risks that affect the income-earning power of the insured person, property risks, and liability risks that cover losses resulting from social interactions. Not all pure risks are covered by private insurers.
### 4.2 ) Types Of Insurance
There are two broad categories of insurance:
#### 1. Life Insurance
#### 2. General insurance
**Life Insurance –** The insurance policy whereby the policyholder (insured) can ensure financial freedom for their family members after death. It offers financial compensation in case of death or disability.
While purchasing the life insurance policy, the insured either pay the lump-sum amount or makes periodic payments known as premiums to the insurer. In exchange, of which the insurer promises to pay an assured sum to the family if insured in the event of death or disability or at maturity.
Depending on the coverage, life insurance can be classified into the below-mentioned types:
+ Term Insurance: Gives life coverage for a specific time period.
+ Whole life insurance: Offer life cover for the whole life of an individual
+ Endowment policy: a portion of premiums go toward the death benefit, while the remaining is invested by the insurer.
+ Money back Policy: a certain percentage of the sum assured is paid to the insured in intervals throughout the term as survival benefit.
+ Pension Plans: Also called retirement plans are a fusion of insurance and investment. A portion from the premiums is directed towards retirement corpus, which is paid as a lump-sum or monthly payment after the retirement of the insured.
+ Child Plans: Provides financial aid for children of the policyholders throughout their lives.
+ ULIPS – Unit Linked Insurance Plans: same as endowment plans, a part of premiums go toward the death benefit while the remaining goes toward mutual fund investments.
**General Insurance** – Everything apart from life can be insured under general insurance. It offers financial compensation on any loss other than death. General insurance covers the loss or damages caused to all the assets and liabilities. The insurance company promises to pay the assured sum to cover the loss related to the vehicle, medical treatments, fire, theft, or even financial problems during travel.
General Insurance can cover almost anything, and everything but the five key types of insurances available under it are –
+ Health Insurance: Covers the cost of medical care.
+ Fire Insurance: give coverage for the damages caused to goods or property due to fire.
+ Travel Insurance: compensates the financial liabilities arising out of non-medical or medical emergencies during travel within the country or abroad
+ Motor Insurance: offers financial protection to motor vehicles from damages due to accidents, fire, theft, or natural calamities.
+ Home Insurance: compensates the damage caused to home due to man-made disasters, natural calamities, or other threats
### What is the difference between “P&C” and “Life Insurance”?
Insurance companies provide a guaranteed payment for an unforeseen future event. The party receiving the payment, the insured, pays a premium for this guarantee. Insurance companies also generate investment income by investing the cash premiums received in the financial markets.
Although this basic concept remains constant throughout the sector, the types of events that are covered by each insurance company vary and so do the associated risks and risk mitigation strategies.
Property and casualty (P&C) insurance, also known as general insurance, is a type of insurance that covers damages to property or a business. This umbrella term covers multiple types of insurance such as auto insurance, home insurance, commercial insurance, and marine insurance. The main risk associated with this sector is underwriting risk which is the risk that income from policies may not be sufficient to cover claims and is usually managed using reinsurance.
Life insurance covers the risk of the death of a policyholder. The policy owner selects beneficiaries who will receive payments upon the policy owner’s death in exchange for premiums paid to the insurance company. The main risk in this sector is longevity risk, which has to do with the uncertainty of the estimated life expectancy of the policyholders. To manage this risk, life insurance policies generally also provide retirement products, which carry the inverse risk to longevity risk, known as mortality risk.
Beyond the above-mentioned differences, the time horizon between the two varies significantly as well; P&C insurance lasts for a few years, whereas life insurance policies last for decades.

### P&C Insurance Risks
One of the major risks that P&C insurance companies face are catastrophes – hurricanes, floods, and earthquakes. These create underwriting risks where the premiums may not be sufficient to cover future claims. Stop-loss reinsurance is important for managing this risk. Stop-loss reinsurance is a type of excess of loss reinsurance wherein the reinsurer is liable for the insured’s losses incurred over a certain period (usually a year) that exceed a specified dollar amount or percentage of some business measure, such as earned premiums written, up to the policy limit.
P&C insurers also face market risk through their investment portfolio, where changes in market conditions can affect their investment portfolio. This is managed by having a diverse portfolio which reduces the effect of adverse movements within single assets within the portfolio.
### Life Insurance Risks
Actuaries working for life insurance companies use mortality tables to make informed assumptions of the expected lifespan of their policyholders. Life insurance companies subsequently face longevity risk and mortality risk.
Longevity risk refers to the chance that life expectancies and actual survival rates exceed projections or pricing assumptions, resulting in greater-than-anticipated cash flow needs on the part of insurance companies. This risk is usually managed with reinsurance and by diversifying the range of products offered.
The mortality risk is the risk that an insurance company can suffer financially because too many of their life insurance policyholders die before their expected lifespans. To mitigate against this risk, life insurance companies sell retirement products. Retirement products provide a natural hedge against mortality risk.
Life insurance companies also face interest rate risk, a type of market risk, on both investment portfolios and future payments to beneficiaries. Since payments are guaranteed long-term, the present value of the payments are affected by changes in future interest rates. This risk is managed by ensuring that cash flow from their investments are well-matched with expected pay-outs on policies. This is achieved by making investments that have similar long-term time horizons to the insurance products.
### 4.3 ) What Is Liability Insurance?
Liability insurance is an insurance product that provides protection against claims resulting from injuries and damage to other people or property. Liability insurance policies cover any legal costs and payouts an insured party is responsible for if they are found legally liable. Intentional damage and contractual liabilities are generally not covered in liability insurance policies.
Unlike other types of insurance, liability insurance policies pay third parties, and not policyholders.
#### How Liability Insurance Works
Liability insurance is critical for those who are liable and at fault for injuries sustained by other people or in the event that the insured party damages someone else's property. As such, liability insurance is also called third-party insurance. Liability insurance does not cover intentional or criminal acts even if the insured party is found legally responsible. Policies are taken out by anyone who owns a business, drives a car, practices medicine or law—basically anyone who can be sued for damages and/or injuries. Policies protect both the insured and third parties who may be injured as a result of the policyholder's unintentional negligence.
For instance, most states require that vehicle owners have liability insurance under their automotive insurance policies to cover injury to other people and property in the event of accidents. A product manufacturer may purchase product liability insurance to cover them if a product is faulty and causes damage to the purchasers or another third party. Business owners may purchase liability insurance that covers them if an employee is injured during business operations. The decisions doctors and surgeons make while on the job also require liability insurance policies.
#### Types of Liability Insurance
Business owners are exposed to a range of liabilities, any of which can subject their assets to substantial claims. All business owners need to have an asset protection plan in place that's built around available liability insurance coverage.
##### Here are the main types of liability insurance:
+ **Employer’s liability and workers' compensation** is mandatory coverage for employers which protects the business against liabilities arising from injuries or the death of an employee.
+ **Product liability insurance** is for businesses that manufacture products for sale on the general market. Product liability insurance protects against lawsuits arising from injury or death caused by their products.
+ **Indemnity insurance** provides coverage to protect a business against negligence claims due to financial harm resulting from mistakes or failure to perform.
+ **Director and officer liability coverage** covers a company's board of directors or officers against liability if the company should be sued. Some companies provide additional protection to their executive team even though corporations generally provide some degree of personal protection to their employees.
+ **Umbrella liability policies** are personal liability policies designed to protect against catastrophic losses. Coverage generally kicks in when the liability limits of other insurance are reached.
+ **Commercial liability insurance** is a standard commercial general liability policy also known as comprehensive general liability insurance. It provides insurance coverage for lawsuits arising from injury to employees and the public, property damage caused by an employee, as well as injuries suffered by the negligent action of employees. The policy may also cover infringement on intellectual property, slander, libel, contractual liability, tenant liability, and employment practices liability.
+ **Comprehensive general liability policies** are tailor-made for any small or large business, partnership or joint venture businesses, a corporation or association, an organization, or even a newly acquired business. Insurance coverage includes bodily injury, property damage, personal and advertising injury, medical payments, and premises and operations liability. Insurers provide coverage for compensatory and general damages for lawsuits but not punitive damages.
### Definition of Administrative services only (ASO)
ASO is a self-funded employee benefits plan structure made by the employer. The employer is then exclusively liable for all of the financial and legal aspects of the plan.
Most often the employer hires an outside firm to administer the plan and process claims and payments. For instance, a firm can hire an insurance company in order to assess and proceed claims under its employee health plan, while retaining the responsibility to pay the claims itself.
#### Benefits and usage of ASO
In an ASO, yearly funding levels are based on actual paid claims, while fully-insured plans are affected by the insurer's evaluation of anticipated claims for a chosen year. When given claims come to be less then anticipated, employers keep the surplus and that can be reinvested. However, when budgeted amounts are exceeded the employer is held responsible.
ASO plans are convinient for benefits such as short term disability, extended health and dental care, but may not be suitable for life insurance and high extended health care plans. It is up to the employer to weigh the risks and benefits of how different ASO arrangements may impact their organizations.
### 4.4) Characteristics of an Ideally Insurable Risk
Private insurers generally insure only pure risks. However, some pure risks are not privately insurable. From the viewpoint of a private insurer, an insurable risk ideally should have certain characteristics. There are ideally six characteristics of an insurable risk:
+ **There must be a large number of exposure units.**
+ **The loss must be accidental and unintentional.**
+ **The loss must be determinable and measurable.**
+ **The loss should not be catastrophic.**
+ **The chance of loss must be calculable.**
+ **The premium must be economically feasible.**
Most insurance providers only cover pure risks, or those risks that embody most or all of the main elements of insurable risk. These elements are "due to chance," definiteness and measurability, statistical predictability, lack of catastrophic exposure, random selection, and large loss exposure.
#### Due to Chance
An insurable risk must have the prospect of accidental loss, meaning that the loss must be the result of an unintended action and must be unexpected in its exact timing and impact.
The insurance industry normally refers to this as "due to chance." Insurers only pay out claims for loss events brought about through accidental means, though this definition may vary from state to state. It protects against intentional acts of loss, such as a landlord burning down his or her own building.
#### Definiteness and Measurability
For a loss to be covered, the policyholder must be able to demonstrate a definite proof of loss, normally in the form of bills in a measurable amount. If the extent of the loss cannot be calculated or cannot be fully identified, then it is not insured. Without this information, an insurance company can neither produce a reasonable benefit amount or premium cost.

#### Statistically Predictable
Insurance is a game of statistics, and insurance providers must be able to estimate how often a loss might occur and the severity of the loss. Life and health insurance providers, for example, rely on actuarial science and mortality and morbidity tables to project losses across populations.(the word morbidity refers to the incidence or prevalence of a disease in a specific population or location (sometimes called the morbidity rate), while the word mortality refers to relative frequency of deaths in a specific population or location (sometimes called the mortality rate).)
#### Not Catastrophic
Standard insurance does not guard against catastrophic perils. It might be surprising to see an exclusion against catastrophes listed among the core elements of an insurable risk, but it makes sense given the insurance industry's definition of catastrophic, often abbreviated as "cat."
There are two kinds of catastrophic risk. The first is present whenever all or many units within a risk group, such as the policyholders in that class of insurance, are all be exposed to the same event. Examples of this kind of catastrophic risk include nuclear fallout, hurricanes, or earthquakes.
The second kind of catastrophic risk involves any unpredictably large loss of value not anticipated by either the insurer or the policyholder. Perhaps the most infamous example of this kind of catastrophic event occurred during the terrorist attacks on Sept. 11, 2001.
Some insurance companies specialize in catastrophic insurance, and many insurance companies enter into reinsurance agreements to guard against catastrophic events. Investors can even purchase risk-linked securities, called "cat bonds," which raise money for catastrophic risk transfers.
#### Randomly Selected and Large Loss Exposure
All insurance schemes operate based on the law of large numbers. This law states there must be a sufficient large number of homogeneous exposures to any specific event in order to make a reasonable prediction about the loss related to an event.
A second related rule is that the number of exposure units, or policyholders, must also be large enough to encompass a statistically random sample of the overall population. This is designed to prevent insurance companies from only spreading risk among those most likely to generate a claim, as might occur under adverse selection.

[Table of Content](#0.1)
___
# 5.) What Is the Morbidity Rate?
Morbidity rate refers to the rate at which a disease or illness occurs in a population and can be used to determine the health of a population and its healthcare needs. Illnesses can range from acute to chronic, long-lasting conditions.
Morbidity rates are also used in actuarial professions, such as health insurance, life insurance, and long-term care insurance, to determine the premiums to charge customers. This rate shouldn't be confused with the mortality rate, another metric used to highlight the frequency of death in a given population.
[Table of Content](#0.1)
___
# 6.) What Is the Law of Large Numbers?
The law of large numbers, in probability and statistics, states that as a sample size grows, its mean gets closer to the average of the whole population. This is due to the sample being more representative of the population as the sample become larger.
#### Understanding the Law of Large Numbers
The law of large numbers can refer to two different topics. First, in statistical analysis, the law of large numbers can be applied to a variety of subjects. It may not be feasible to poll every individual within a given population to collect the required amount of data, but every additional data point gathered has the potential to increase the likelihood that the outcome is a true measure of the mean.
The law of large numbers does not mean that a given sample or group of successive samples will always reflect the true population characteristics, especially for small samples. This also means that if a given sample or series of samples deviates from the true population average, the law of large numbers does not guarantee that successive samples will move the observed average toward the population mean.
Second, the term "law of large numbers" is sometimes used in business in relation to growth rates, stated as a percentage. It suggests that, as a business expands, the percentage rate of growth becomes increasingly difficult to maintain. This is because the underlying dollar amount is actually increasing even if the growth rate as a percentage is to remain constant.

#### Law of Large Numbers and Statistical Analysis
If a person wanted to determine the average value of a data set of 100 possible values, he is more likely to reach an accurate average by choosing 20 data points instead of relying on just two. This is because there is greater probability of the two data points being outliers or non-representative of the average, while there is lower probability in all 20 data points being non-representative.
For example, if the data set included all integers from one to 100, and sample-taker only drew two values, such as 95 and 40, he may determine the average to be approximately 67.5. If he continued to take random samplings up to 20 variables, the average should shift towards the true average as he considers more data points.
#### Law of Large Numbers and Central Limit Theorem
In statistical analysis, the law of large numbers is related to the central limit theorem. The central limit theorem states that as the sample size increases, the sample mean will be evenly distributed. This is often depicted as a bell-shaped curve where the peak of the curve depicts the mean and even distributions of sample data fall to the left and right of the curve.
In a related manner, the law of large numbers also states that data is refined as the sample grows. However, the law of large numbers more closely relates to the center of the bell curve. The law of large numbers indicates that as a sample size increases, the mean of the sample will more closely resemble the mean of the population. Therefore, the law of large numbers relates to the peak (the mean) of a curve, while the central limit theorem relates to the distribution of a curve.
#### Law of Large Numbers in Business Example
In fiscal year 2020, Tesla reported automotive sales (not gross sales) of $24.604 billion. The next year, the company reported $44.125 billion, an increase of roughly 79%.
As electric vehicles are an emerging market and Tesla is beginning to finally experience economies of scale, the company is started to experience success very quickly.
The law of large numbers indicates that as Tesla continues to grow, it will become harder for the company to maintain this level of productivity. For example, assuming a steady growth rate of the next several years, it becomes quickly apparent that Tesla simply cannot maintain its current growth trajectory due to the underlying dollar values becoming unreasonable.
[Table of Content](#0.1)
___
# 7.) Insurance obligation
what it means, is that on any date, the sum of (a) all Reimbursement Amounts, (b) all accrued and unpaid premium and charges for "Unutilized Credit Limit Capacity" under the Insurance Policy and (c) all other accrued and unpaid amounts then due and payable to the Insurer under the Insurance Policy and any other Transaction Document.
**Obligation #1:** An insurer must treat its insured’s interests with the same consideration it gives its own interests. This means that a claims adjuster must give the policy holder the benefit of the doubt. The claims adjuster should be looking for reasons to find coverage, not for reasons to deny coverage. The claims adjuster should be looking for reasons to pay the claim, not reasons to deny it. Unfortunately, sometimes insurance companies lose sight of this fundamental rule.
**Obligation #2:** The claims adjuster has a duty to help the policy holder with the claim. A claims adjuster should help explain coverage and available benefits to the policy holder and should take other steps to help bring the claim to a prompt and fair conclusion. Claims adjusters should not view the process as insurance company versus policy holder.
**Obligation #3:** The insurer must promptly and fairly investigate every claim. This obligation may best be illustrated by an example. A firm handled a case where the claims adjuster for the client’s insurance company did not obtain medical records, interview witnesses, or evaluate the claim in any meaningful way for a period of 2 ½ years. They did not promptly and fairly investigate the client’s claim.
**Obligation #4:** If payment is owed, an insurer must promptly pay the claim. In Wisconsin, an insurer must pay a claim that is owed within 30 days, or the insurer may be subject to paying the policy holder 12 percent interest per year. Even though this is the law, there is no good reason for an insurance company to hold payment for 30 days if it owes benefits under a policy.
**Obligation #5:** If the insurer denies the claim, it must give an explanation to the policy holder. An insurance company cannot simply refuse payment of a policy holder’s claim without an explanation. A policy holder has a right to know the reasons that payment of a claim is being denied so that he or she can respond appropriately.
**Obligation #6:** The insurer must disclose significant facts to its policy holder. Throughout its investigation into a claim, the insurer must tell the policy holder about significant facts or circumstances it uncovers. An insurer has investigators and others experienced in the claims process. They are in the best position to conduct an investigation. In fact, if a policy holder takes certain actions or compromises an investigation, an insurer may argue that coverage has been voided. Because of the unique nature of the insurer/insured relationship and the realities of the claims process, an insurance company must disclose significant facts to its policy holder.
Again, insurance companies must treat their insureds fairly and reasonably. If an insurer violates one or more of its obligations to you, may have committed bad faith.
#### What is the meaning by obligation?
An act of making oneself responsible for doing something(as a promise or contract) that requires one to do something.
#### What is an example of a obligation?
For example, if you owe or will owe money to anybody, that is one of your financial obligations. Almost any form of payment or financial security represents a financial obligation.
[Table of Content](#0.1)
___
# 8.) What Is Reinsurance?
Reinsurance is also known as insurance for insurers or stop-loss insurance. Reinsurance is the practice whereby insurers transfer portions of their risk portfolios to other parties by some form of agreement to reduce the likelihood of paying a large obligation resulting from an insurance claim.
The party that diversifies its insurance portfolio is known as the ceding party. The party that accepts a portion of the potential obligation in exchange for a share of the insurance premium is known as the reinsurer.
### 8.1 ) How Reinsurance Works
Reinsurance allows insurers to remain solvent(having assets in excess of liabilities; able to pay one's debts) by recovering some or all amounts paid to claimants. Reinsurance reduces the net liability on individual risks and catastrophe protection from large or multiple losses. The practice also provides ceding companies, those that seek reinsurance, the capacity to increase their underwriting capabilities in terms of the number and size of risks.
According to the Insurance Information Institute, Hurricane Andrew caused $15.5 billion in damage in Florida in 1992, causing seven U.S. insurance companies to become insolvent(unable to pay debts owed).
By spreading risk, an individual insurance company can take on clients whose coverage would be too great of a burden for the single insurance company to handle alone. When reinsurance occurs, the premium paid by the insured is typically shared by all of the insurance companies involved.
If one company assumes the risk on its own, the cost could bankrupt or financially ruin the insurance company and possibly not cover the loss for the original company that paid the insurance premium.
For example, consider a massive hurricane that makes landfall in Florida and causes billions of dollars in damage. If one company sold all the homeowners insurance, the chance of it being able to cover the losses would be unlikely. Instead, the retail insurance company spreads parts of the coverage to other insurance companies (reinsurance), thereby spreading the cost of risk among many insurance companies.
Insurers purchase reinsurance for four reasons: To limit liability on a specific risk, to stabilize loss experience, to protect themselves and the insured against catastrophes, and to increase their capacity. But reinsurance can help a company by providing the following:
+ **Risk Transfer:** Companies can share or transfer specific risks with other companies.
+ **Arbitrage:** Additional profits can be garnered by purchasing insurance elsewhere for less than the premium the company collects from policyholders.
+ **Capital Management:** Companies can avoid having to absorb large losses by passing risk; this frees up additional capital.
+ **Solvency Margins:** The purchase of surplus relief insurance allows companies to accept new clients and avoid the need to raise additional capital.
+ **Expertise:** The expertise of another insurer can help a company obtain a higher rating and premium.

#### Reinsurance occurs when multiple insurance companies share risk by purchasing insurance policies from other insurers to limit their own total loss in case of disaster. Described as "insurance of insurance companies" by the Reinsurance Association of America, the idea is that no insurance company has too much exposure to a particularly large event or disaster

[Table of Content](#0.1)
___
A deductible is the amount of money that you are responsible for paying toward an insured loss. When a disaster strikes your home or you have a car accident, the deductible is subtracted, or "deducted," from what your insurance pays toward a claim. Deductibles are how risk is shared between you, the policyholder, and your insurer.
Generally speaking, the larger the deductible, the less you pay in premiums for an insurance policy. A deductible can be either a specific dollar amount or a percentage of the total amount of insurance on a policy.
#### How deductibles work
A specific amount would be subtracted from your claim payment if you have a dollar amount deductible. For example, if your policy states a $500 deductible, and your insurer has determined that you have an insured loss worth $10,000, you would receive a claims check for $9,500.
Percentage deductibles generally only apply to homeowners policies and are calculated based on a percentage of the home’s insured value. Therefore, if your house is insured for $100,000 and your insurance policy has a 2 percent deductible, $2,000 would be deducted from any claim payment. In the event of the $10,000 insurance loss, you would be paid $8,000. For a $25,000 loss, your claim check would be $23,000.
Note that with auto insurance or a homeowners policy, the deductible applies each time you file a claim. There are exceptions to this practice in Florida and Louisiana, where hurricane deductibles are applied once per season rather than for each storm.
Deductibles generally apply to property damage, not to the liability portion of homeowners or auto insurance policies. For example, with a homeowners policy, a deductible would apply to property damaged in a rogue outdoor grill fire; however, there would be no deductible against the policy's liability portion if a burned guest made a medical claim or sued.
#### Raising your deductible can save money
One way to save money on a homeowners or auto insurance policy is to raise the deductible. Therefore, if you're shopping for insurance, ask about the options for deductibles when comparing policies.
Increasing your auto insurance's dollar deductible from $200 to $500 can reduce optional collision and comprehensive coverage premium costs. Going to a $1,000 deductible may save you even more. Most homeowners and renters insurers offer a minimum $500 or $1,000 deductible, and raising the deductible to more than $1,000 can save on the cost of the policy.
Of course, remember that you'll be responsible for the deductible in the event of loss, so make sure that you're comfortable with the amount.
#### Homeowners disaster deductibles
Standard homeowners insurance covers wind and hail damage from storms and hurricanes. Flood and earthquake policies are purchased separately. But each of these disasters has its own deductible rules. If you live in an area with a high risk for one of these natural disasters, understand how much deductible you will need to pay if a catastrophe strikes.
Start here, check your policies and speak to your insurance professional to learn exactly how your deductibles work.
+ **Hurricane deductibles:** In hurricane-prone states, special deductibles may apply for homeowners insurance claims when the cause of damage is attributable to a hurricane. Whether a hurricane deductible applies to a claim depends on the specific "trigger" selected by the insurance company. These triggers vary by state and insurer and usually apply when the National Weather Service (NWS) officially names a tropical storm, declares a hurricane watch or warning, or defines a hurricane's intensity in terms of wind speed. Hurricane deductibles are generally higher than other homeowners' policy deductibles and usually take the form of a percentage of the policy limits. In some states, policyholders can choose to pay a higher premium in return for a traditional dollar deductible; however, in high-risk coastal areas, insurers may make the percentage deductible mandatory.
+ **Wind/hail deductibles** work in a similar way to hurricane deductibles and are most common in places that typically experience severe windstorms and hail. These include Midwestern states (like Ohio) and around Tornado Alley (including Texas, Oklahoma, Kansas, and Nebraska). Wind/hail deductibles are most commonly paid in percentages, typically from 1 percent to 5 percent.
+ **Flood insurance** offers a range of deductibles. If you have—or are considering buying—flood insurance, make sure you understand your deductible. Flood insurance deductibles vary by state and insurance company and are available in dollar amounts or percentages. Also, you can choose one deductible for your home's structure and another for the contents of your home. Note that your mortgage company may require that your flood insurance deductible under a certain amount to help ensure you will be able to pay it).
+ **Earthquake insurance** has percentage deductibles that range from 2 percent to 20 percent of the replacement value of your home, depending on location. Insurers in states with a higher than average risk of earthquakes (such as Washington, Nevada, and Utah) often set minimum deductibles at around 10 percent. In California, the basic California Earthquake Authority (CEA) policy includes a deductible that is 15 percent of the replacement cost of the main home structure and starting at 10 percent for additional coverages (such as on a garage or other outbuildings).
## 9.1 ) Aggregating Specific Deductible
An aggregate deductible is the limit deductible a policyholder would be required to pay on claims during a given period of time. Aggregate deductibles are most likely to be features of product liability policies or policies that might result in a large number of claims during a certain time period.
##### How an Aggregate Deductible Works
The draw of an aggregate deductible policy feature is that it puts a cap on the amount the insured has to pay. Manufacturers purchase product liability insurance to protect themselves from claims resulting from damages caused by their products. It is especially valuable for products that can cause significant damages if not manufactured correctly, such as medicines and automobiles, and with products that are sold in high volumes, such as toys.
While policyholders may have product liability insurance batch clauses, not all states will allow the policyholder to treat all claims as if they were part of the same occurrence. If each claim is considered independent, then the policyholder will have to pay the deductible for each claim, even if the deductible is greater than the claim amount. This essentially creates a situation in which the policyholder is not insured.
##### What It Is
With this feature, employers pay reduced stop-loss premiums in exchange for taking on more risk of a set dollar
amount, known as the Aggregate Specific Deductible. This is in addition to the Specific Deductible that is already
in place. The Aggregate Specific Deductible covers the entire group and must be satisfied before an employer can
get reimbursed.
##### How It Works
This example shows an employer with a:
■ $200,000 Specific Deductible
■ $60,000 Aggregate Specific Deductible
Three employees each have claims that exceed the $200,000 Specific Deductible.

##### Example of an Aggregate Deductible
For example, a canning company is notified that some of its products are making the consumers sick. The company’s per occurrence deductible is $10,000, but it also has an aggregate deductible that designates that it does not have to pay more than $100,000 in deductibles in a given year.

The total number of claims reaches 1,000, and each claim valued at $5,000. Without an aggregate deductible, the company would be responsible for the entire claim, and would ultimately have to pay out $5,000,000 ($5,000 claim value x 1,000 claims). The aggregate deductible, however, limits the company’s total deductible to $100,000.
**The aggregating specific deductible** goes by many names. You may have heard the term referred to as the aggregating specific corridor or more affectionately the Agg Spec or even simply the ASD. Regardless of what you call it, the ASD can be a critical element in your Stop Loss contract. When an aggregating specific deductible is employed, the client assumes additional liability in exchange for a lower premium. The ASD is a set dollar amount that is used to cover a single claimant or many claimants, who exceed the specific deductible. In some instances, a group’s claims may not reach their agg spec. In this case, the group would save the premium dollars they would have spent had they opted not to pursue an ASD. When the total claims paid meets the value of the ASD, the stop loss carrier assumes liability for any claims exceeding the deductible.
For example, a group opts to add a $100,000 aggregating specific deductible to their stop loss contract, which has a $150,000 specific deductible for each member. As in a standard stop loss contract, the group pays for all medical expenses up to $150,000 for all members. The first claims that exceed the $150,000 specific deductible, whether from a single member or several, are paid by the group’s aggregating specific deductible funds. Claims exceeding the $150,000 spec will continue to be paid by the group’s funds until the $100,000 has been paid out. At this point, the carrier will begin issuing reimbursements for additional claims.
#### Aggregate Deductibles and Health Insurance
Aggregate deductibles are also used in family health insurance policies. Under an aggregate deductible family health insurance plan, the total family deductible must be paid out-of-pocket before health insurance starts paying for the health care services incurred by any family member.
With an aggregate deductible, there is no embedded deductible for each individual family member to meet. Aggregate deductible family health insurance may carry a lower monthly premium, but the coverage doesn't take effect until the full family deductible is paid out of pocket, which can be much higher than individual embedded deductibles for each family member.
[Table of Content](#0.1)
___
# 10.) What Is Coinsurance?
Coinsurance is the percentage of covered medical expenses you pay after you've met your deductible. Your health insurance plan pays the rest. For example, if you have an "80/20" plan, it means your plan covers 80% and you pay 20%—up until you reach your maximum out-of-pocket limit.
Still, coinsurance only applies to covered services. If you have expenses for services that the plan doesn't cover, you'll be responsible for the entire bill. If you're not sure what your plan covers, review your benefits booklet or call your plan provider.
Coinsurance is the amount, generally expressed as a fixed percentage, an insured must pay toward a covered claim after the deductible is satisfied. It is common in health insurance. Some property insurance policies also contain coinsurance provisions. In this case, coinsurance is the amount of coverage that the property owner must purchase for a structure.

#### How Coinsurance Works
A coinsurance provision is similar to a copayment, or "copay," provision, except that copays require the insured to pay a set dollar amount at the time of the service, and coinsurance is a percentage amount.
One of the most common coinsurance breakdowns is the 80/20 split. Under the terms of an 80/20 coinsurance plan, the insured is billed for 20% of medical costs, while the insurer pays the remaining 80%.
However, these terms only apply after the insured has reached the policy's out-of-pocket deductible amount. Also, most health insurance policies include an out-of-pocket maximum that limits the total amount the insured pays for care in a given period.

#### Example of Coinsurance
Here's how it typically works: Assume you take out a health insurance policy with an 80/20 coinsurance provision, a $1,000 out-of-pocket deductible, and a $5,000 out-of-pocket maximum. Unfortunately, you require outpatient surgery early in the year that costs $5,500. Because you have not yet met your deductible, you must pay the first $1,000 of the bill. After meeting your $1,000 deductible, you are then only responsible for 20% of the remaining $4,500, or $900. Your insurance company will cover 80%, the remaining balance.
If you require another expensive procedure later in the year, your coinsurance provision takes effect immediately because you have previously met your annual deductible. Also, because you have already paid a total of $1,900 out-of-pocket during the policy term, the maximum amount that you will be required to pay for services for the rest of the year is $3,100.
After you reach the $5,000 out-of-pocket maximum, your insurance company is responsible for paying up to the maximum policy limit, or the maximum benefit allowable under a given policy.
[Table of Content](#0.1)
___
# 11.) What Are Copays?
A co-pay, short for co-payment, is a fixed amount that a healthcare beneficiary pays for covered medical services. The remaining balance is covered by the person’s insurance company.
Co-pays typically vary for different services within the same plans, particularly when they involve services that are considered essential or routine and others that are considered less routine or in the domain of a specialist.
Co-pays are typically lower for standard doctor visits than for seeing specialists. Co-pays for emergency room visits tend to be the highest.
Copays (or copayments) are set amounts you pay to your medical provider when you receive services. Copays typically start at $10 and go up from there, depending on the type of care you receive. Different copays usually apply to office visits, specialist visits, urgent care, emergency room visits, and prescriptions.
Your copay applies even if you haven't met your deductible yet. For example, if you have a $50 specialist copay, that's what you'll pay to see a specialist—whether or not you've met your deductible.

#### Copay and Coinsurance Example
To help explain copays and coinsurance, here's a simplified example.
Say you have an individual plan (no dependents) with a $3,000 deductible, $50 specialist copays, 80/20 coinsurance, and a maximum out-of-pocket limit of $6,000.
You go for your annual checkup (which is free because it's a preventive service) and mention that your shoulder has been hurting. Your doctor sends you to an orthopedic specialist (for a $50 copay) to take a closer look.
That specialist recommends an MRI to find out what's going on. The MRI costs $1,500. You pay the entire amount because you haven't met your deductible yet.
As it turns out, you have a torn rotator cuff and need surgery to fix it. The surgery costs $7,000. You've already paid $1,500 for the MRI, so you need to pay $1,500 of the surgery bills to meet your deductible and have the coinsurance kick in. After that, your share is 20%—which, in this example, is $1,100. All in, your torn rotator cuff costs you $4,100.
[Table of Content](#0.1)
___
# 12.) Coinsurance vs. Copay: What's the Difference?
Coinsurance and copays are both important terms for understanding the costs of health insurance. These and other out-of-pocket costs affect how much you'll pay for the healthcare you and your family receive.



[Table of Content](#0.1)
___
# 13.) Co-pay vs. Deductible: What’s the Difference?
Co-pays and deductibles are features of health insurance plans. They involve payment on the part of the insured, but the amount and frequency differ.

#### What Are Deductibles?
A deductible is a fixed amount that a patient must pay each year before their health insurance benefits begin to cover the costs.
After meeting a deductible, beneficiaries typically pay co-insurance—a certain percentage of costs—for any services covered by the plan. They continue to pay the co-insurance until they meet their out-of-pocket maximum for the year.

### Preventive Services
In most cases, preventive services are covered at 100%—meaning that the patient doesn’t owe anything for the appointment. Plans offered through the Patient Protection and Affordable Care Act pay in full for routine checkups and other screenings considered preventive, such as mammograms and colonoscopies for people over a certain age.
### Real-Life Example
Suppose a patient has a health insurance plan with a $30 co-pay to visit a primary care physician, a $50 co-pay to see a specialist, and a $10 co-pay for generic drugs.
The patient pays these fixed amounts for those services regardless of what the services actually cost. The insurance company pays the remaining balance (the “covered amount”). Therefore, if a visit to the patient’s endocrinologist (a specialist) costs $250, the patient pays $50 and the insurance company pays $200.
Now suppose the same patient has a $2,000 annual deductible before insurance starts to pay, and 20% co-insurance after that.
In March, he sprains his ankle playing basketball, and treatment costs $300. He pays the full cost because he has yet to meet his deductible. In May, he has back problems, which cost $500 to treat. Again, he pays the full cost.
In August, he breaks his arm playing touch football, and the bill for his hospital visit comes to $3,500. On this bill, the patient pays $1,200—the balance of his deductible. Once he meets the deductible, he also pays 20% (his co-insurance amount). In this case, that would be an additional $460 (20% of $2,300—the difference between the deductible and the hospital visit).
#### Does Coinsurance Count Toward the Deductible?
No. Coinsurance is the portion of healthcare costs that you pay after your spending has reached the deductible. For example, if you have a 20% coinsurance, then your insurance provider will pay for 80% of all costs after you have met the deductible.
Do All Health Insurance Plans Have Copays and Coinsurance?
No. Some healthcare plans might not require customers to pay a copay for certain medical services, although these plans will typically come with higher premiums. On the other end, a catastrophic health plan with a very high deductible might pay as much as 100% of many preventive expenses, without coinsurance.
#### Are Copays and Coinsurance Tax-Deductible?
Healthcare costs such as copays, coinsurance, and premiums may be tax-deductible if they exceed 7.5% of your adjusted gross income. If your healthcare expenses exceed that threshold, the amount over 7.5% can be deducted.
[Table of Content](#0.1)
___
# 14.) What Are Out-of-Pocket Maximums?
Out-of-pocket expenses are healthcare costs that are not covered by insurance, for example, if your spending has not yet reached your plan deductible. The out-of-pocket maximum is the maximum amount of out-of-pocket expenses you will have to pay in one year.
When you reach your out-of-pocket maximum, your health insurance plan covers 100% of all covered services for the rest of the year. Any money you spend on deductibles, copays, and coinsurance counts toward your out-of-pocket maximum. However, premiums don't count, and neither does anything you spend on services that your plan doesn't cover.
Like deductibles, you might have two out-of-pocket limits—an individual one and a family one. Under the Affordable Care Act, the highest allowable out-of-pocket maximum is set at $8,550 for individual coverage and $17,100 for family coverage.
[Table of Content](#0.1)
___
# 15.) What’s a High-Deductible Health Plan?
A high-deductible health plan is an inexpensive health insurance plan with low premiums but a very high deductible. Because they may come with significant out-of-pocket expenses, these plans are popular for young, healthy workers with low routine medical expenses who are worried about catastrophic healthcare events.
An additional benefit of high-deductible plans is the Health Savings Account, which is only available to workers with an HDHP. These savings accounts are tax-free, so long as the money is used for qualified medical expenses.
[Table of Content](#0.1)
___
# 16.) In-Network vs. Out-of-Network
Some plans have two sets of deductibles, copays, coinsurance, and out-of-pocket maximums: one for in-network providers and one for out-of-network providers.
In-network providers are doctors or medical facilities with which your plan has negotiated special rates. Out-of-network providers are everything else—and they are generally much more expensive.
Keep in mind that in-network doesn't necessarily mean close to where you live. You could have a North Carolina plan and see an in-network provider at the Cleveland Clinic in Ohio.
Whenever possible, be sure you're using in-network providers for all of your healthcare needs. If there are certain doctors and facilities you'd like to use, be sure they're part of your plan's network. If not, it might make financial sense to switch plans during the next open enrollment period.
[Table of Content](#0.1)
___
# 17.) What is Inpatient vs. Outpatient Care?
The terms “inpatient” and “outpatient” have very different meanings in the health care world. Knowing the difference between inpatient vs. outpatient care can give you the edge when it comes to managing your health care, choosing a health plan, and planning ahead for out-of-pocket medical expenses related to outpatient or inpatient care.
## What’s the main difference between inpatient and outpatient care?
Generally speaking, inpatient care requires you to stay in a hospital and outpatient care does not. The big difference is whether you need to be hospitalized or not.
What is inpatient care?
Inpatient care is care provided in a hospital or other type of inpatient facility, where you are admitted, and spend at least one night—sometimes more—depending on your condition.
## As an inpatient:
- You are under the care of doctors, nurses, and other types of health care professionals within a hospital.
- You are often admitted to a particular service, such as Neurology, Cardiology, Orthopedics, Oncology, General Surgery, etc., depending on what you are being treated for.
- You may be an inpatient due to surgery, illness, childbirth, or traumatic injury. There are inpatient facilities and hospitals for substance use and mental health illness, as well.
- Your inpatient stay may have been planned ahead—such as a knee replacement surgery or childbirth.
- Your stay may have been the result of an emergency or unplanned illness or injury, such as a heart attack or serious car accident.
- You are in need of medicine, care, monitoring, and medical treatment—the kind that’s provided by around-the-clock medical staff.
- Once a doctor decides you no longer require inpatient care, you are discharged from the facility. Discharge notes often include instructions to follow up with various doctors, take prescribed medications, and even receive outpatient services, if needed.
## What is outpatient care?
Outpatient care—the kind that you don’t have to stay in a hospital for—can vary greatly. Other than an annual check-up or blood test, almost any other kind of care can be defined as outpatient. These may be diagnostic tests, treatments, or other types of procedures.
**`Outpatient care may be provided in a hospital, as well as a walk-in clinic, an outpatient surgery center, and even your doctor’s office.`**
### What determines if you need inpatient vs. outpatient care?
Whether you need outpatient or inpatient care is often determined by the type of care you require. Intensive care, around-the-clock care, major surgery, and treatment for a serious illness, are examples of medical situations that would require you to be admitted to the hospital.
On the other hand, there are plenty of minor surgeries, procedures, medical screenings, and treatments that do not require overnight stays or hospitalization.
### What are some examples of inpatient care?
Types of inpatient care include:
- Serious illness, such as flu, stroke, heart attack
- Traumatic injury
- Severe burns
- Serious mental health issues, treatment for substance use disorder, and overdoses
- Chronic diseases, such as cancer and chronic obstructive pulmonary disease (COPD), that require specialized treatment and ongoing care
- Some cosmetic procedures requiring extensive plastic surgery or reconstruction
### What are some examples of outpatient care?
#### Types of outpatient care include:
- Medical screenings such as mammogram, colonoscopy, and endoscopy
- Oral surgeries and other dental procedures, such as extractions, implants, root canal, and gum grafts
- Minor surgeries and procedures that don’t require advanced medical care, such as laser surgery, hand or foot surgery, mole removal, and Lasik eye surgery
- Certain types of treatment used for ongoing or long-term illnesses, such as dialysis and chemotherapy
## What are the costs for outpatient vs. inpatient?
The costs for inpatient care can add up. In addition to the cost for the treatment or surgery you’re getting, there are many other costs associated with being cared for in a hospital, including:
- Administrative costs
- Pharmacy costs
- Lab tests
- Costs for nurses, radiologists, technicians, and specialists
Equipment and supplies that contribute to your care while you’re there
And more
### The costs for outpatient care are typically considerably less than inpatient care. You often have some control over the costs too. For example:
Costs for diagnostic radiology and imaging can vary greatly, so shop around for things like MRIs, PET, and CT scans to see how you can best keep your cost low.
When it comes to needing unplanned medical care, understanding the difference between urgent care and the ER can ensure you don’t pay more than you need to.
There are some outpatient screenings and procedures that are considered preventive care and covered by your plan. Things like a routine mammogram and colonoscopy are often covered 100% by your health plan.*
Learn more about how to pay less for out-of-pocket medical costs.
### Do you have coverage for inpatient vs. outpatient health care?
Your health plan covers you for medical care, in general, regardless of whether it’s outpatient or inpatient. And some outpatient care may be covered 100% as part of your preventive care. Things like a routine mammogram or routine colonoscopy are examples of outpatient preventive care.
### Here’s how your plan covers you for care and services:
- You pay for care and services until you meet your plan deductible.
- Once you meet your deductible, your health plan kicks in to start sharing costs as part of coinsurance. For example, you may pay 20% of the cost for services and your plan may pay the remaining 80%.
- If you hit your out-of-pocket maximum for the year—that’s the most you’re required to pay out-of-pocket—then your health plan will start paying 100% of the costs for your care.
- Understanding the difference between inpatient vs. outpatient care and services can help give you more control over your health care. It gives you more control when you’re comparing health plans, when you’re planning ahead for a medical procedure or treatment, and anticipating costs for inpatient or outpatient services.
[Table of Content](#0.1)
___
# 18.) Stop-Loss Insurance 101
Stop-Loss Insurance Coverage is defined as a layer of coverage that provides reimbursement to self-insured employers for catastrophic claims exceeding predetermined levels. This coverage is purchased by employers who self-fund their employee benefit plan so that they don’t have to assume all of the liability for losses arising from an extremely high medical claim.
**In simple terms:**
Stop-loss insurance (also known as excess insurance) is a product that provides protection against catastrophic or unpredictable losses. It is purchased by employers who have decided to self-fund their employee benefit plans, but do not want to assume 100% of the liability for losses arising from the plans. Under a stop-loss policy, the insurance company becomes liable for losses that exceed certain limits called deductibles.
There are many different options for stop-loss coverages and contracts. Before you draft a contract or schedule a meeting with your insurance carrier, here is a brief introduction to the different stop-loss options, contracts, and terms.
#### 18.1 ) There are two types of self-funded insurance:
**Specific Stop-Loss:** This form of stop-loss coverage protects a self-insured employer against large claims incurred by a single individual. Under a specific stop-loss policy, the employer will be reimbursed when claims for an individual exceed a specified deductible. This is protection against abnormal severity of a single claim rather than abnormal frequency of claims in total. Specific stop-loss is also known as individual stop-loss.
**Aggregate Stop-Loss:** This form of stop-loss provides a ceiling to the amount that an employer would pay in expenses on the entire plan, on an aggregate basis, during a contract period. Under this policy, the insurance carrier reimburses the employer after the end of the contract period for aggregate claims.
It provides a ceiling on the dollar amount of eligible expenses that an employer would pay, in total, during a contract period. **The carrier reimburses the employer after the end of the contract period for aggregate claims.**
This coverage ensures that a catastrophic claim (specific stop-loss) or numerous claims (aggregate stop-loss) do not drain the financial reserves of a self-funded plan. Aggregate stop-loss protects the employer against claims that are higher than expected. If total claims exceed the aggregate limit, the stop-loss insurer covers the claims or reimburses the employer.
There are a number of variations available for each of these coverages, and there are employers that protect their plan with a combination of both specific and aggregate stop-loss coverages. Here is a quick overview of what specific and aggregate stop-loss policies may look like for your organization.
#### Specific Stop-Loss At A Glance
Under a Specific Stop-Loss Policy, an employer may elect for a maximum liability per person on their benefits plan. If the claims exceed that point, the stop-loss policy will reimburse the employer for the claims in excess of that amount.
For example, if an employer elects that their maximum liability per person on their benefits plan for that policy year be $100,000, and a specific claimant exceeds that liability and their total claims are $102,000, the stop-loss policy will reimburse them for claims in excess of that amount, the $2,000.
The maximum liability employers take on can range from $10,000 to $1 million, and generally fall within 3 to 6 percent of the expected annual claim amount.
Under a specific stop-loss policy, employers can be eligible to receive coverage for both medical and prescription drugs.
The contracts that specify these details can be written in a variety of ways depending on the insurance carrier.
Maximum liability per person is determined by employers and their insurance carriers, and the amount an insurance carrier is willing to be liable for is subject to their specific policies.
#### Aggregate Stop-Loss At A Glance
Aggregate stop-loss insurance is held for self-funded insurance plans for which an employer assumes the financial risk of providing healthcare benefits to its employees. In practical terms, self-funded employers pay for each claim as it is presented instead of paying a fixed premium to an insurance carrier for a fully insured plan. Stop-loss insurance is similar to purchasing high-deductible insurance. The employer remains responsible for claim expenses under the deductible amount.
Stop-loss insurance differs from conventional employee benefit insurance. Stop-loss only covers the employer and provides no direct coverage to employees and health plan participants.
Aggregate Stop-Loss protects against higher than anticipated claims for the entire plan. If the total paid claims exceed the established point amount, the carrier will reimburse the employer for the excess.
The point at which the insurance carrier is liable is determined by the carrier, and is generally derived from the enrollment on the employer’s insurance plan and on the aggregate attachment factor. The process for determining the aggregate attachment factor is as follows:
+ First, the stop-loss carrier determines the average expected monthly claims PEPM based on the employer’s history.
+ Then, this figure is multiplied by a percentage ranging from 110%-150%.
+ That determined amount is then multiplied by the enrollment on a monthly basis to establish the aggregate deductible.
#### How Aggregate Stop-Loss Insurance Is Used
Aggregate stop-loss insurance is used by employers as coverage for risk against a high value of claims. Aggregate stop-loss insurance comes with a maximum level for claims. When a maximum threshold is exceeded, the employer no longer needs to make payments and may receive some reimbursements.
Aggregate stop-loss insurance can either be added to an existing insurance plan or purchased independently. The threshold is calculated based on a certain percentage of projected costs (called attachment points)—usually 125% of anticipated claims for the year.
An aggregate stop-loss threshold is usually variable and not fixed. This is because the threshold fluctuates as a percentage of an employer’s enrolled employees. The variable threshold is based on an aggregate attachment factor which is an important component in the calculation of a stop-loss level.
As is the case with high deductible plans, most stop-loss plans will have relatively low premiums. This is because the employer is expected to cover over 100% of the value of claims they receive.
##### An example of deriving the Aggregate Stop-Loss coverage is as follows:
+ First, the employer and stop-loss carrier establish the average expected monthly claims, for this example $300 PEPM.
+ This figure is then multiplied by a percentage usually ranging between 110%-150%, for this example 150%.
+ From these calculations, the aggregate attachment factor is established as $450.
+ This attachment factor is then multiplied by the employees enrolled, for this example 1,000. This calculation equals out to a total amount of $450,000.
+ That amount is the aggregate deductible for the month, and if that enrollment remains the same for the whole year, the annual aggregate will total $5,400,000.
+ Assuming enrollment stays level and the contract term is a year, the maximum out of pocket claims for this employer would be $5,400,000.
+ If claims exceed this amount, say $5,500,000, the stop-loss carrier will be liable to pay that excess, in this example $100,000.
+ $300 x 150% = $450
+ $450 x 1,000 = $450,000
+ $450,000 x 12 = $5,400,000
##### **Note:**
Enrollment can potentially vary per month. Due to enrollment variance, aggregate stop-loss coverage may have either a monthly deductible or an annual deductible.
With a monthly deductible, the amount an employer must pay could change every month. With an annual deductible, the amount the employer must pay would be summed for the year and usually based on estimates from the initial month of coverage. Many stop-loss plans will offer an annual deductible that is slightly lower than the summation of deductibles over 12 months.

#### Why Invest in a Stop-Loss Insurance Policy?
By incorporating stop-loss into their insurance policy, these self-funded employers are limiting their risk, safeguarding themselves against high claims, and impacting their bottom-line by opting out of expensive, traditional insurance policies.
### Understanding Aggregate Stop Loss vs. Specific Stop Loss
Aggregate stop loss and specific stop loss are kind of like rain boots and umbrellas. They work in slightly different ways to address the same problem. You can choose to use both types or just one depending on what kind of protection you need, both using both is the best way to limit your exposure in a storm.
Stop loss coverage creates a ceiling for how much a self-insured employer has to pay for high claims, and aggregate and specific are two forms of this coverage. Self-insured employers who want to manage risk may use both types of coverage to achieve maximum protection from high-value claims.
#### What Aggregate Stop Loss Does
Aggregate stop loss puts a cap on the amount that a self-insured employer has to pay across an entire plan year. Having an aggregate stop loss policy helps the employer budget for its healthcare costs with some accuracy, since this policy lets the employer put a dollar figure on its maximum potential liability for the plan year.
Working with a third-party administrator or insurer, a client with this type of policy will set an aggregate deductible that’s based on its total expected monthly claims and its risk tolerance. That number is multiplied by a percentage (commonly 125 percent) to determine the plan’s aggregate attachment point. The company pays for its claims, and at the end of the policy period, it’s reimbursed for any claims that exceeded the aggregate attachment point.
#### What Specific Stop Loss Does
While aggregate stop loss coverage protected a self-funded employer against higher-than-expected costs across its entire plan, specific stop loss puts a cap on the amount that the employer will pay for any one individual claim. This type of protection shields the employer from great risk if any plan members incur catastrophic claims. An employee who needs a heart transplant, or has a serious accident and requires weeks of hospitalization, could easily incur hundreds of thousands of dollars in medical bills. Cancer, certain chronic conditions and childbirth complications are all pretty routine diagnoses that can cause individual employees’ claims to skyrocket.
Like with aggregate stop loss policies, a specific stop loss policy has a specific deductible. There are a number of factors involved in setting this number. Some self-funded plans have a specific deductible of $50,000, while others have a $1 million deductible. Somewhere around $200,000 to $300,000 is a pretty typical range. The self-insured employer is responsible for individual claims that fall below the deductible. For claims above the deductible, the employer pays upfront and the stop loss carrier reimburses any portion exceeding that threshold. Specific claims may be reimbursed as soon as the individual’s deductible has been met.
#### Making the Right Choice For You
It’s common for self-insured companies that buy stop loss coverage to choose both aggregate and specific policies. Few companies, outside of major corporations, have adequate resources to absorb whatever claims their members incur. And again, having both specific and aggregate stop loss policies is really useful for projecting costs, so this is a kind of protection that most self-insured employers want. Sometimes employers opt for just specific coverage, or just aggregate coverage, depending on their needs and circumstances.
Just as aggregate and specific deductibles vary widely based on the employer’s needs, so do stop loss premiums. It’s tough to predict exactly what you’ll pay for your policy until you’ve sat down and worked through the options with a plan administrator. Your company’s risk tolerance will play a big role in what you pay for premiums. But if your company already has a budget established you may be able to tailor your plan to meet that budget, without compromising the quality of healthcare your employees receive. Remember, one of the prime benefits of self-funding is that it lets the employer trim waste and pay only for the services its employees receive.
#### Stop-Loss Insurance Contract Terms and Terminology
In order to fully understand stop-loss policies, it is critical to know the different stop-loss contract terms. Stop-loss contracts are written depending on the agreement made between the insurance carrier and employer.
These contracts specify the time period when the insurer is liable to cover claims and by what time employers must pay the claims they are liable for. There are many different term agreements, and which terms an employer is subject to depends on the contract between the employer and the insurance carrier. These different contract terms can include policies such as:
+ **“12/12” Contract:** Under this contract agreement, claims must be incurred and paid during the plan year.
+ **“12/15” Contract:** Under this contract agreement, claims must be incurred during the plan year and paid either during the plan year or during the three months after the end of the plan year.
+ **“15/12” Contract:** Under this contract agreement, claims must be incurred in the three months prior to the end of the plan date and paid during the plan year.
+ **Deductibles:** The limit at which the insurance company becomes liable for paying medical claims.
+ **Disclosure:** An insurance carrier will require the disclosure of known high claimants or high-risk individuals before giving a final quote.
+ **Lasering:** An insurance carrier can place a higher deductible on certain individuals or exclude them from coverage.
[Table of Content](#0.1)
___
Lasering is a common stop loss practice in which an individual participant—based on prior claims experience or known conditions—is covered by the stop loss policy at a higher Specific deductible than the rest of the group. As a result, the employer takes on additional claim risk for the individual in exchange for lower annual premium across the entire plan.
##### 3 reasons to consider lasering:
+ **Long-term savings:** Using lasers to manage anticipated high-cost claims for individual participants helps keep premium costs for the entire plan in check. And mitigating the cost of the current year’s premium sets a lower starting point for any future rate increases, allowing the group to realize long-term savings.
+ **Opportunities for cost-containment solutions:** When a single member or multiple members with similar conditions/diagnoses are projected to incur significant claims costs, employers can work with their administrator to implement cost-savings options for the overall plan.
+ **Potential cost savings for participants:** Adjusting stop loss coverage for individuals rather than raising rates across the entire group helps reduce overall expenses for the plan. If the group’s medical benefits include premium cost-share, these savings can then be passed on to plan participants, thereby reducing their contribution requirements.
[Table of Content](#0.1)
___
### 20.) Definition of Technical Provisions
Technical provisions represent the amount that an insurer( a person or company that contracts to indemnify another in the event of loss or damage) requires to fulfil its insurance obligations and settle all expected commitments to policyholders and other beneficiaries arising over the lifetime of the insurer's portfolio of insurance contracts.
#### A starting point
+ Within a prudent insurer, management would record details of
+ Amount paid on each claim , both total paid and the history of payments
+ Amount and date of the case reserve or case estimate, being the difference between payments made and the estimated ultimate or final loss for each claim either
+ an estimate based of the judgement of an experienced person within the insurer , typically for medium and large claims,
+ an average claim amount, typically for smaller claims or as an initial amount until the claim is reviewed
+ These case estimates or incurred loss (i.e. paid loss plus case estimate) made be used to prioritise or allocate resources
+ However the total of the case estimates also represents an estimate of technical provisions in respect of claims notified.
+ The importance of technical provisions to the maintenance of solvency has led to the development of other estimation methods.
#### Key Featues of Technical provisions
From Summary of IAIS positions
+ comprise two components
+ the current estimate of the costs of meeting the insurance obligations (Current Estimate)
+ margin for risk (Margin over Current Estimate or MOCE)
+ undertaken on a market-consistent basis
+ any valuation or modelling assumptions should be based
+ on current data
+ on the most credible current assumptions
+ Similar insurance obligations with similar risk profiles should result in the determination of similar values for technical provisions
+ The credit standing of an insurer should not be considered in the valuation of its insurance liabilities
+ The amount of the technical provisions should be consistent with an exit of the insurer, in the sense that any transfer of insurance obligations , based on the technical provisions, to another newly licenced insurer would result in the receiving insurer being capable of settling the obligations.
+ a prudent, reliable and objective manner to allow comparison across insurers worldwide
[Table of Content](#0.1)
___
# 21.) What Is a Health Reimbursement Arrangement (HRA)?

A health reimbursement arrangement (HRA) is an employer-funded plan that reimburses employees for qualified medical expenses and, in some cases, insurance premiums. Employers are allowed to claim a tax deduction for the reimbursements they make through these plans, and reimbursement dollars received by employees are generally tax-free.

### How a Health Reimbursement Arrangement (HRA) Works
A health reimbursement arrangement is a plan set up by an employer to cover medical expenses for its employees. The employer decides how much it will put into the plan, and the employee can request reimbursement for actual medical expenses incurred up to that amount. All employees in the same class must receive the same HRA contribution.
An HRA is not an account. Therefore, employees cannot withdraw funds in advance and then use them to pay medical expenses. Instead, they must incur the expense first, then have it reimbursed. Reimbursement at the time of service is possible if the employer provides an HRA debit card.
An employee who uses up all the allocated funds in the HRA before year-end will have to cover any subsequent health bills out-of-pocket or with the funds in a flexible spending account (FSA), also known as a flexible spending arrangement, when available, or a health savings account (HSA) for employees who have a high-deductible health plan (HDHP)

### Types of HRAs
There are a few kinds of health reimbursement arrangements.
Qualified Small Employer Health Reimbursement Arrangement (QSEHRA)
A Qualified Small Employer Health Reimbursement Arrangement (QSEHRA) is a health coverage subsidy plan for employees working for businesses that employ less than 50 full-time workers. Also known as a small business HRA, a QSEHRA can be used to offset health insurance coverage or repay medical expenses that would be otherwise uncovered.
The yearly limits are set by the Internal Revenue Service (IRS). For 2022, a company with a QSEHRA can reimburse individual employees for up to $5,450 per year and employees that have families for up to $11,050 per year.
In 2023, the limits change to $5,850 per individual and $11,800 per family.
The money that is reimbursed is tax-free for the employees and tax-deductible for the employers.
Individual Coverage HRA (ICHRA)
An Individual Coverage HRA (ICHRA) is relatively new, having only been available since January 2020. Previously, HRAs could not be used to pay individual health insurance premiums. But as of January 2020, the government allows employers to offer their employees a new type of HRA called an individual coverage HRA—instead of group health insurance.
Employees can use these HRAs to buy their own comprehensive individual health insurance with pretax dollars either on or off the Affordable Care Act's health insurance marketplace. Individual coverage HRAs can also reimburse employees for qualified health expenses such as copayments and deductibles.
Whether or not your ICHRA makes you eligible for a premium tax credit to help pay for health insurance coverage under the Affordable Care Act depends on whether your employer's ICHRA meets minimum standards for so-called "affordability," and whether you choose to opt-in or opt-out of the coverage.
Excepted Benefit HRAs (EBHRA)
In addition, employers that continue to offer traditional group health insurance can offer Excepted Benefit HRAs (EBHRA) to reimburse employees for up to $1,950 a year in qualified medical expenses.
Employees can enroll in an "excepted benefit HRA" even if they decline group health insurance coverage, but they cannot use the funds to buy comprehensive health insurance. They can, however, use the funds to pay for short-term health insurance, dental and vision insurance premiums, and qualified medical expenses.
### Benefits of Health Reimbursement Arrangements
HRAs can be used to pay for qualified medical expenses, which include prescription medications, insulin, an annual physical exam, crutches, birth control pills, meals paid for while receiving treatment at a medical facility, care from a psychologist or psychiatrist, substance abuse treatment, transportation costs incurred to get medical care, and much more.


### Health Reimbursement Arrangements vs. Other Arrangements
An employee with both an FSA and an HRA—and an expense that is eligible to be reimbursed through both plans—can't choose which will cover the expense. Instead, the costs will be reimbursed by the plan that the employer has set up to pay first. When this primary plan has been depleted, the second plan will be used to cover any subsequent eligible medical expenses that are reported for reimbursement.
Here's a closer look at two other options for funding out-of-pocket medical expenses.
#### FSA
A flexible spending arrangment (FSA) is funded using a portion of an employee's pre-tax salary.
In contrast to an HRA, each employee determines how much money should go into these arrangements annually—up to $2,850 in 2022 and $3,050 in 2023.
Unused funds in HRAs may be carried over to the following year according to the employer's discretion.
Unused FSA funds generally cannot be used in the next plan year, although an employer may offer either a short grace period (2.5 months) or allow up to $610 to be carried over.
### HSA
Compared to an HRA, a health savings account (HSA) is a fully vested tax-advantaged account that is not subject to forfeiture if funds remain in the account at the end of the year. An HSA is paired with a high-deductible health plan (HDHP) to pay for medical and dental expenses. The employee or employer funds the account and, like an FSA, cannot be used to pay insurance premiums. Unlike HRAs and FSAs, employees can keep their HSAs if they change employers.
### How Can I Use HRA Funds?
Your employer determines the types of medical expenses that an HRA can be used for. Some plans can only reimburse services in your health plan, while others might include dental, vision, or pharmacy services.
HRAs often, but do not always, reimburse other expenses such as copays, hospital expenses, medical equipment, eyeglasses, or routine doctor's visits.
In addition, the IRS also excludes certain other expenses as being unqualified. For example, expenses that do not qualify as necessary medical expenses include teeth whitening, maternity clothes, funeral services, health club membership fees, controlled substances, childcare for a healthy baby, medication from other countries, and non-prescription medications.
### HRAs Are Not Portable
HRA Funding and Portability
The health reimbursement arrangement is funded solely by the employer, which also decides the maximum annual contribution for each employee’s HRA. Employers determine how much to contribute to employees’ HRAs, except that all workers in the same class of employees must receive the same contribution, as noted above. Workers who are older or who have dependents may receive more.
Any HRA money unspent by year-end may be rolled over to the following year, although an employer may set a maximum rollover limit that can be carried over from one year to the next.
Furthermore, if an employee is terminated or leaves the company to work for another firm, the HRA does not go with them. That makes it different from an HSA—health savings account—which is portable.
### HRA Tax Advantages
As a benefit to employers, reimbursements through the HRA are 100% tax-deductible.
As an alternative to more expensive traditional healthcare, an employer may use an HRA to cover the health costs of several classes of employees.
In addition, since employers fully fund the plans, they offer predictability, allowing employers to anticipate their approximate maximum expense for HRA health benefits for the year.
Employees may use the arrangement to pay for a wide range of medical expenses not covered by their health insurance policies. Depending on the HRA type, they may also use it for medical, dental, or vision insurance premiums.
Furthermore, reimbursements are tax-free up to a maximum amount for a coverage period. Some businesses may offer employees the added advantage of other employer-provided health benefits, such as an FSA, in conjunction with an HRA.
### Frequently Asked Questions
What Is a HRA in Health Insurance?
A health reimbursement arrangement (HRA) is an employer's plan to cover employee medical expenses.
How Does a HRA Work?
The employer determines the amount of money that will go into the plan, and the employee can ask to be reimbursed for qualified medical expenses up to the designated amount. Employers can take a tax deduction for the reimbursements made through these plans, and the reimbursements given to employees are usually tax-free.
### What Is a HRA vs. a HSA?
A health reimbursement arrangement (HRA) is a benefit used to pay employees back in tax-free money for certain qualified medical expenses and health coverage premiums.
A health savings account (HSA) is a tax-advantaged account used by individuals covered under a high-deductible health plan (HDHP) looking to save up to cover the cost of qualified medical expenses.
### Can I Cash out My HRA?
No. HRA money that hasn't been used by the end of the year can usually be rolled over to the following year, with an employer determining the maximum amount that can be carried from one year to another.
### What Qualifies for HRA Reimbursement?
Examples of medical and dental expenses considered necessary might be an annual check-up, prescriptions, or substance abuse treatment.
[Table of Content](#0.1)
___
# 22.) Health Savings Account (HSA)
## What Is a Health Savings Account (HSA)?
A Health Savings Account (HSA) is a tax-advantaged account created for or by individuals covered under high-deductible health plans (HDHPs) to save for qualified medical expenses. Contributions are made into the account by the individual or their employer and are limited to a maximum amount each year. The contributions are invested over time and can be used to pay for qualified medical expenses, such as medical, dental, and vision care and prescription drugs.

## How an HSA Works
As mentioned above, people with HDHPs can open HSAs. Individuals with HDHPs may qualify for HSAs, and the two are usually paired together. To qualify for an HSA, the taxpayer must meet eligibility standards established by the Internal Revenue Service (IRS). An eligible individual is someone who:
- Has a qualified HDHP
- Has no other health coverage
- Is not enrolled in Medicare
- Is not claimed as a dependent on someone else’s tax return
The maximum contribution for an HSA in 2022 is $3,650 for an individual ($3,850 for 2023) and $7,300 for a family ($7,750 in 2023).
The annual limits on contributions apply to the total of the amounts contributed by both the employer and the employee. Individuals age 55 or older by the end of the tax year can make catch-up contributions of an additional $1,000 to their HSAs.
An HSA can also be opened at certain financial institutions. Contributions can only be made in cash, while employer-sponsored plans can be funded by the employee and their employer. Any other person, such as a family member, can also contribute to the HSA of an eligible individual. Self-employed or unemployed individuals may also contribute to an HSA, provided that they meet the eligibility requirements.
Individuals who enroll in Medicare can no longer contribute to an HSA as of the first month of enrollment.However, they can receive tax-free distributions for qualified medical expenses.
## HSA Special Considerations
HDHPs have higher annual deductibles (the plan pays nothing until you reach these amounts in out-of-pocket expenses) but lower premiums than other health plans. The financial benefit of an HDHP’s low-premium and high-deductible structure depends on your personal situation.
The minimum deductible required to open an HSA is $1,400 for an individual or $2,800 for a family for the 2022 tax year ($1,500 and $3,000, respectively, for 2023). The plan must also have an annual out-of-pocket maximum of $7,050 for self-coverage for the 2022 tax year ($7,500 for 2023) and $14,100 for families for the 2022 tax year ($15,000 for 2023). These maximums cap your out-of-pocket expenses.
When an individual pays qualified medical expenses equal to a plan’s deductible amount, additional qualified expenses are divided between the individual and the plan. For instance, the insurer covers a percentage of the qualified expenses per the contract (usually 80% to 90%), while the plan holder pays the remaining 10% to 20% or a specified co-pay.
Using this guide, an individual with an annual deductible of $1,500 (in 2023) and a medical claim of $3,500 pays the first $1,500 to cover the annual deductible. The insured pays 10% to 20% of the remaining $2,000, while the insurance company covers the rest.
Once the annual deductible is met in a given plan year, the plan typically covers any additional medical expenses, except for any uncovered costs under the contract, such as co-pays. The insured can withdraw money accumulated in an HSA to cover these out-of-pocket expenses.
## Advantages
Employer and individual contributions by payroll deduction to an HSA are excluded from the employee’s taxable income. An individual’s direct contributions to an HSA are 100% tax deductible from the employee’s income. Earnings in the account are also tax free. However, excess contributions to an HSA incur a 6% tax and are not tax deductible.
13
Distributions from an HSA are tax free, provided that the funds are used for qualified medical expenses as outlined by the IRS. Distributions used for medical expenses covered under the HDHP plan are included in determining if the HDHP’s deductible has been met.
You can also use the money in your HSA to invest in stocks and other securities, potentially allowing for higher returns over time.
## Disadvantages
The most obvious key drawback is that you need to be a good candidate for an HDHP. In addition, you must have a high-deductible plan, lower insurance premiums, or be affluent enough to afford the high deductibles and benefit from the tax advantages.
Individuals who fund their own HSAs, whether through payroll deductions or directly, should be financially capable of setting aside an amount that would cover a substantial portion of their HDHPs’ deductibles. Individuals without enough spare cash to set aside in an HSA may find the high deductible amount burdensome.
HSAs also come with filing requirements regarding contributions, specific rules on withdrawals, distribution reporting, and a record-keeping burden that may be difficult to maintain.
[Table of Content](#0.1)
___
# 23.) Preferred Provider Organization (PPO)
## What Is a Preferred Provider Organization (PPO)?
A preferred provider organization (PPO) is a popular health insurance plan designed for individuals and families. PPOs involve networks that are made up of contracted medical professionals and health insurance companies. Healthcare facilities and practitioners, known as preferred providers, offer services to the insurer's plan policyholders at reduced rates. Plan participants receive the maximum PPO benefit when they visit in-network healthcare professionals and are also offered coverage when they see out-of-network providers.

## How Preferred Provider Organizations (PPOs) Work
A preferred provider organization is a managed-care network consisting of medical professionals and facilities, such as primary and specialty physicians, hospitals, and other healthcare professionals, who contract with insurance providers to render services to subscribed participants. These are plan participants or consumers who are covered by the insurer's healthcare plan.
Plans negotiate fees and schedules for services with healthcare professionals and facilities. As such, the agreed-upon rate is typically lower than their usual charges. In exchange for reduced rates, insurers pay the PPO a fee to access the network of providers.
PPO participants are free to use the services of any provider within their network. They are encouraged, but not required, to name a primary care physician, and don't need referrals to visit a specialist. Subscribers may go out of network for coverage but it often comes at a higher cost.
## The Costs of a PPO Plan
There are a number of costs associated with PPOs, and premiums tend to be higher than other types of insurance plans. PPO plans tend to charge higher premiums because they are costlier to administer and manage. Participants are generally responsible for copayments, which are paid directly to the provider at each visit. There are also deductibles that patients must meet before the plans start kicking in and paying claims in full.
As noted above, plan participants are also allowed to visit out-of-network facilities, usually at a higher cost. These charges are based on a reasonable and customary fee schedule. If those claims made by these healthcare providers exceed the reasonable and customary fees for services rendered, coverage may not apply or, most commonly, the excess charge is passed on to the patient.
One important point to note is the degree of flexibility associated with the higher cost of PPOs. These plans offer more options than others available on the market. PPO networks are typically large, with providers in many cities and states. Choosing a provider or accessing one in urgent situations provides value to participants.
## Preferred Provider Organization (PPO) vs. Health Maintenance Organization (HMO)
In contrast to PPOs, health maintenance organization (HMO) plans require participants to receive healthcare services from an assigned provider. This is a primary care doctor who coordinates the insured's care. Both programs allow the insured to seek specialist care but under an HMO plan, the designated primary care physician must provide a referral to a specialist.
As noted above, PPO plans charge higher premiums than almost every other plan for the convenience, accessibility, and freedom they offer. This includes a wider choice of hospitals and doctors. Plans with the lowest/fewest out-of-pocket expenses, such as those with low deductibles and low copayments, have higher premiums. The elevated premium cost is due to the insurer absorbing more of the associated costs. Conversely, lower-premium alternatives translate into higher out-of-pocket costs for the insured and lower costs for the insurer.
PPO plans come with more comprehensive coverage, including many services that other managed-care programs might exclude or for which they would charge an additional premium.
PPO plans have historically been the preferred choice among employer group participants. However, today, participants want more options for managed healthcare. Therefore, many employers offer HMO plans as well. Because HMO premiums are less expensive, some participants favor HMO plans for their affordability, although services and freedoms typically associated with PPO plans are often restricted.
## How Do PPO Deductibles Work?
A health insurance deductible is an amount you must pay out of pocket for medical services each year; after you've met it, your insurance coverage kicks in. PPO plans may have two different annual deductibles. One applies to providers in the PPO network, the other—usually a larger sum—to providers outside the network. The latter is larger because the PPO wants to encourage you to stay in network, using its preferred providers.
## What Are Disadvantages of PPO Plans?
PPO plans tend to be more expensive than other managed-care options. They typically have higher monthly premiums and out-of-pocket costs, like deductibles. You often have both coinsurance and copays. This is the tradeoff for the flexibility PPOs provide, of letting you use providers both within and outside the PPO system, without needing referrals.
The costs for coinsurance and deductibles can be different for in-network and out-of-network providers and services. Some may find it onerous to have more responsibility for managing and coordinating their own care without a primary care doctor.
## What Is the Difference Between a PPO and a POS?
The biggest difference between PPO and POS plans is generally flexibility. Both plans cover you whether you use providers and facilities in or out of the network. However, a POS requires you to have a primary care physician and get referrals from them if you want to see a specialist or anyone else. PPOs don't. Costs are another consideration. PPOs tend to be more expensive than POS plans—the premiums are higher and they usually come with deductibles that must be met before your coverage begins.
[Table of Content](#0.1)
___
# 24.) Preferred Provider Organization (PPO)
## What Is a Health Maintenance Organization (HMO)?
An individual who needs to secure health insurance may find a variety of insurance providers with unique features. One type of insurance provider that is popular on the Health Insurance Marketplace is a health maintenance organization (HMO), an insurance structure that provides coverage through a network of physicians.
There are several key differences between HMO plans and preferred provider organization (PPO) plans. With an HMO plan, your primary care physician (PCP) will refer you to specialists, and you must stay within a network of providers to receive coverage. On the other hand, HMO plans typically have lower premiums than PPO plans.

## How a Health Maintenance Organization (HMO) Works
HMOs provide health insurance coverage for a monthly or annual fee. An HMO limits member coverage to medical care provided through a network of doctors and other healthcare providers who are under contract with the HMO. These contracts allow for premiums to be lower than for traditional health insurance—since the healthcare providers have the advantage of having patients directed to them. However, they also add additional restrictions to the HMO’s members.
When deciding whether to choose an HMO plan, you should take into consideration the cost of premiums, out-of-pocket costs, any requirements you may have for specialized medical care, and whether it’s important to you to have your own primary care physician (PCP).
An HMO is an organized public or private entity that provides basic and supplemental health services to its subscribers. The organization secures its network of health providers by entering into contracts with PCPs, clinical facilities, and specialists. The medical entities that enter into contracts with the HMO are paid an agreed-upon fee to offer a range of services to the HMO’s subscribers. The agreed payment allows an HMO to offer lower premiums than other types of health insurance plans while retaining a high quality of care from its network.
The HMO as it exists today was established under the Health Maintenance Organization Act of 1973. Signed by then-President Richard Nixon, the law clarified the definition of HMOs as “a public or private entity organized to provide basic and supplemental health services to its members.” The law further requires that plans provide insured individuals with basic healthcare in exchange for regular, fixed premiums that are established “under a community rating system.”
## Rules for HMO Subscribers
HMO subscribers pay a monthly or annual premium to access medical services in the organization’s network of providers, but they are limited to receiving their care and services from doctors within the HMO network. However, some out-of-network services, including emergency care and dialysis, can be covered under the HMO.
Those who are insured under an HMO may have to live or work in the plan’s network area to be eligible for coverage. In cases where a subscriber receives urgent care while out of the HMO network region, the HMO may cover the expenses. But HMO subscribers who receive nonemergency, out-of-network care have to pay for it out of pocket.
In addition to low premiums, there are typically low or no deductibles with an HMO. Instead, the organization charges a co-pay for each clinical visit, test, or prescription. Co-pays in HMOs are typically low—usually, $5, $10, or $20 per service—thereby minimizing out-of-pocket expenses and making HMO plans affordable for families and employers.
## Role of the Primary Care Physician (PCP)
The insured party must choose a PCP from the network of local healthcare providers under an HMO plan. A PCP is typically an individual’s first point of contact for all health-related issues. This means that an insured person cannot see a specialist without first receiving a referral from their PCP.
However, certain specialized services, such as screening mammograms, do not require referrals. Specialists to whom PCPs typically refer insured members are within the HMO coverage, so their services are covered under the HMO plan after co-pays are made. If a PCP leaves the network, subscribers are notified and are required to choose another PCP from within the HMO plan.
## HMO Regulation
HMOs are regulated by both states and the federal government. The McCarran-Ferguson Act of 1945 established that even though the insuring or provision of healthcare may be national in scope, the regulation of insurance should be largely left to the states. Likewise, the Health Maintenance Organization Act provides that HMO or health service plans are regulated by the states. As a result of these two federal statutes, much of the task of health insurance regulation is left to the states.
That said, the federal government does maintain some oversight on health maintenance organizations. The 2010 Dodd-Frank Act created the Federal Insurance Office (FIO), which can monitor all aspects of the insurance industry. Similarly, the Affordable Care Act of 2010 created an agency charged with overseeing insurance agencies, called the Center for Consumer Information and Insurance Oversight (CCIIO).
## HMO vs. Preferred Provider Organization (PPO)
A preferred provider organization (PPO) is a medical care plan in which health professionals and facilities provide services to subscribed clients at reduced rates. PPO medical and healthcare providers are called preferred providers.
PPO participants are free to use the services of any provider within their network. Out-of-network care is available, but it costs more to the insured. In contrast to PPO plans, HMO plans require that participants receive healthcare services from an assigned provider. PPO plans usually have deductibles, while HMO plans usually do not.
Both programs allow for specialist services. However, the designated PCP must provide a referral to a specialist under an HMO plan. PPO plans are the oldest and—due to their flexibility and relatively low out-of-pocket costs—have been the most popular managed healthcare plans. That has been changing, however, as plans have reduced the size of their provider networks and taken other steps to control costs.
## HMO vs. Point-of-Service (POS)
A point-of-service (POS) plan is like an HMO plan in that it requires a policyholder to choose an in-network PCP and get referrals from that doctor if they want the plan to cover a specialist’s services. A POS plan is also like a PPO plan in that it still provides coverage for out-of-network services, but the policyholder has to pay more for those services than if they used in-network providers.
However, a POS plan will pay more toward an out-of-network service if the policyholder gets a referral from their PCP than if they don’t secure a referral. The premiums for a POS plan fall between the lower premiums offered by an HMO and the higher premiums of a PPO.
POS plans require the policyholder to make co-pays, but in-network co-pays are often just $10 to $25 per appointment. POS plans also do not have deductibles for in-network services, which is a significant advantage over PPOs.
Also, POS plans offer nationwide coverage, which benefits patients who travel frequently. A disadvantage is that out-of-network deductibles tend to be high for POS plans, so patients who use out-of-network services will pay the full cost of care out of pocket until they reach the plan’s deductible. However, a patient who never uses a POS plan’s out-of-network services probably would be better off with an HMO because of its lower premiums.
If you don’t travel frequently, you’ll be better off with an HMO plan than a POS plan because of the lower costs.
Advantages and Disadvantages of HMOs
It’s important to weigh the advantages and disadvantages of HMO plans before you choose a plan, just as you would with any other option. We’ve listed some of the most common pros and cons of the program below.
## Advantages of HMOs
The first and most obvious advantage of participating in an HMO is the low cost. You’ll pay fixed premiums on a monthly or annual basis that are lower than traditional forms of health insurance. These plans tend to come with low or no deductibles, and your co-pays are generally lower than other plans. Your out-of-pocket costs will also be lower for your prescription. Billing also tends to be less complicated.
There’s also a very good likelihood that you’ll have to deal with the insurer itself. That’s because you have a PCP who you choose and who is responsible for managing your treatment and care. This professional will also advocate for services on your behalf. This includes making referrals for specialty services for you.
The quality of care is generally higher with an HMO plan. That is because patients are encouraged to get annual physicals and seek out treatment early.
## Disadvantages of HMOs
If you’re paying for an HMO, then you’re restricted on how you can use the plan. You’ll have to designate a doctor, who will be responsible for your healthcare needs, including your primary care and referrals. However, this doctor must be part of the network. This means that you are responsible for any costs incurred if you see someone out of the network, even if there’s no contracted doctor in your area.
You’ll need referrals for any specialists if you want your HMO to pay for any visits. If you need to visit a rheumatologist or a dermatologist, for example, your PCP must make a referral before you can see one for the plan to pay for your visit. If not, you’re responsible for the entire cost.
There are very specific conditions that you must meet for certain medical claims, such as emergencies. For instance, there are usually very strict definitions of what constitutes an emergency. If your condition doesn’t fit the criteria, then the HMO plan won’t pay.

[Table of Content](#0.1)
___
# 25.) Point-of-Service (POS)?
## What Is a Point-of-Service (POS) Plan?
A point-of-service (POS) plan is a type of managed-care health insurance plan that provides different benefits depending on whether the policyholder uses in-network or out-of-network healthcare providers.
A POS plan combines features of the two most common health insurance plans: the health maintenance organization (HMO) and the preferred provider organization (PPO). POS plans represent a small share of the health insurance market. Most policyholders have either HMO or PPO plans.

## How a Point-of-Service (POS) Works
A POS plan is similar to an HMO. It requires the policyholder to choose an in-network primary care doctor and obtain referrals from that doctor if they want the policy to cover a specialist’s services. And a POS plan is like a PPO in that it still provides coverage for out-of-network services, but the policyholder will have to pay more than if they used in-network services.
However, the POS plan will pay more toward an out-of-network service if the primary care physician makes a referral than if the policyholder goes outside the network without a referral. The premiums for a POS plan fall between the lower premiums offered by an HMO and the higher premiums of a PPO.
POS plans require the policyholder to make co-payments, but in-network co-payments are often just $10 to $25 per appointment. POS plans also do not have deductibles for in-network services, which is a significant advantage over PPOs.
POS plans offer nationwide coverage, which benefits patients who travel frequently. A disadvantage is that out-of-network deductibles tend to be high for POS plans. When a deductible is high, it means that patients who use out-of-network services will pay the full cost of care until they reach the plan’s deductible. A patient who never uses a POS plan’s out-of-network services probably would be better off with an HMO because of its lower premiums.

## Disadvantages of POS Plans
Though POS plans combine the best features of HMOs and PPOs, they hold a relatively small market share. One reason may be that POS plans are marketed less aggressively than other plans. Pricing also might be an issue. Though POS plans can be up to 50% cheaper than PPO plans, premiums can cost as much as 50% more than for HMO premiums.
While POS plans are cheaper than PPO plans, plan details can be challenging, the policies can be confusing, and many consumers don’t understand how the associated costs work. Read the plan documents especially carefully—and compare them to other choices—before deciding whether this is the best option.
[Table of Content](#0.1)
___
# 26.) What Is Incurred But Not Reported (IBNR)?
Incurred but not reported (IBNR) is a type of reserve account used in the insurance industry as the provision for claims and/or events that have transpired, but have not yet been reported to an insurance company.
In IBNR situations, an actuary will estimate potential damages, and the insurance company may decide to set up reserves to allocate funds for the expected losses. To an actuary, these types of events and losses are said to have been incurred but not reported.
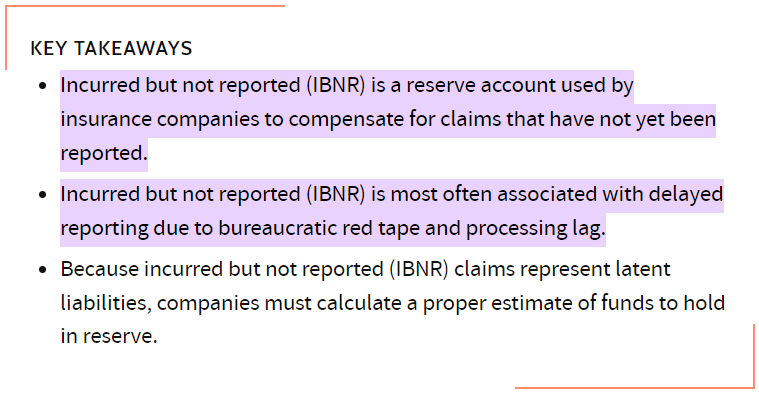
### How Incurred But Not Reported (IBNR) Works
IBNR is frequently used by insurance companies, particularly along the East and Gulf Coasts of the United States (where hurricanes and other natural disasters are common). After a storm hits, actuaries estimate the potential damage to infrastructure and the claims that may be anticipated. Based on this analysis, money is then set aside (in a reserve) to pay for claims. Again, in this example, the actual losses have been incurred, but have not officially been reported.
There are numerous scenarios that can conspire and make it necessary for insurance companies to maintain funding provisions for IBNR claims.
For example, the potential impact of slowly developing occupational disease claims on workers' compensation claims. Such examples include silicosis, asbestosis, and certain cancers determined to be related to occupational exposures. Defective product or product liability claims often have delayed reporting, such as lead-based paint, asbestos insulation, and defective drywall.
Poor environmental practices can also result in delayed reporting of environmental liability claims. Finally, short-term workers compensation injuries and healthcare claims to a group healthcare plan can experience delayed reporting.
It is very important to understand how insurance carriers use IBNR to calculate your account’s performance.
Delayed reporting impacts several types of insurance coverages, which require an IBNR calculation. These include workers' compensation, environmental/pollution, healthcare, general liability, and products liability.
### How IBNR Is Calculated
Determining the right and proper formula for calculating an appropriate IBNR has always been one of the toughest challenges of the insurance industry. Insurance claim variables are non-normally distributed, which makes estimating them problematic–and not getting it right is not without consequence. Inaccurate estimates can project an incorrect view of an insurer’s health and may result in action being taken that could be detrimental to the company.
#### At a minimum, an actuary would likely use this client data to calculate IBNR:
+ Claim amount
+ Claim number
+ Claim paid dates
+ Claim settlement expense
+ Class of business
+ Intimation date
+ Loss date
+ Policy from date
+ Policy number
+ Policy to date
+ Product type
+ Reinsurance paid – a share of the claim amount
+ Reinsurance paid – a share of claim settlement expenses
[Table of Content](#0.1)
___
# 27.) Wholesale and Retail Insurance?
#### Wholesale Insurance
Wholesale insurance is sold to groups that may not be large enough to get typical group coverage. They are essentially provided by companies with fewer than 10 employees. Plans come with individual contracts but generally contain the same provisions for all members of the group. Some companies allow employees to purchase a policy while others pay premiums as part of the employee benefits package.
Wholesale insurance is normally offered by nonadmitted carriers. These providers are also known as surplus line or excess line carriers. These companies don't necessarily have to follow regulations outlined for insurance companies by the state. As such, policies offered by nonadmitted carriers can be risky because they may not guarantee claims if the insurer becomes insolvent.

#### Products for small businesses offered through wholesale insurance vary and generally include the following:
+ Environmental liability products
+ High-risk products for chemical and flammable incidents
+ Pharmaceutical and medical products against product failure
+ Privacy protection products against identity theft
+ Products that are critical to safety for transportation
+ Construction-related structural integrity products
Insurance wholesalers rarely have direct contact with insured parties except when it comes to employee benefit and health plans. Because nonadmitted carriers don't operate under state insurance laws, they have more pricing flexibility to ensure against unusual circumstances such as catastrophic events. While there is a certain risk that comes with some nonadmitted carriers, the fact that they operate outside of state insurance laws shouldn't be a red flag of financial instability. State licensing, filing, and reporting requirements are simply different for these carriers. Larger nonadmitted carriers are usually well-capitalized subsidiaries of major financial services companies.
#### Retail Insurance Markets
The retail insurance market is generally comprised of "licensed producers" generating insurance policies that are underwritten by "admitted carriers." When you're in the market for p/c insurance, in the usual process, your retail agent or broker (producer) finds a policy from insurance carriers licensed to do business in your state. These licensed carriers, called admitted carriers, are under stringent regulatory supervision by your state's Department of Insurance. Insurance producers are also licensed, and are likewise under stringent regulatory supervision by your state's Department of Insurance.
#### Wholesale Insurance Markets
Producers are sometimes unable to find admitted carriers because the risks don't conform to carrier risk guidelines. In other instances, the coverage might entail expertise beyond the capability of the producer.
In these instances, the producer will enlist the help of a wholesale insurance broker/agent to find a carrier, or enlist the help of a broker/agent having specialized capabilities. This new broker/agent, called a surplus line producer, acts as the middleman between the "retail" producer and the carrier with the needed resources, according to IRMI. This new middleman is called a surplus line producer or "wholesaler."
Wholesaler insurance companies must have a surplus lines license because their market is quite unique. Insurance carriers operating in the wholesale market are called "non-admitted carriers." They are typically not licensed by your state's Department of Insurance. They're also called excess and surplus line carriers or "wholesale carriers..
#### Wholesale Insurance vs. Retail Insurance
Wholesale insurance coverage is unlike the retail insurance market. Most individuals are used to the retail insurance market where they buy auto, home, and life insurance. Policies in this market are normally underwritten by carriers who are admitted, or companies that are licensed in the state in which the policy is sold. Admitted carriers are regulated by the state, and broker-agents are also held to regulatory standards by the state as well.
#### How the Wholesale Market Works
The wholesale market provides coverage for risks outside of the risk preference of admitted carriers, according to Sapling. Some wholesalers also provide specialized capabilities such as administering employee benefit and health plans for small businesses or in a particular line of coverage or in a line of coverage that is unusual and/or have greater access to or influence with certain insurance markets, which is especially valuable when dealing with a difficult-to-place risk.
Wholesalers rarely have direct contact with the insured except in instances such as employee benefit and health plans. Because non-admitted carriers don't operate under state insurance laws, they have more pricing flexibility to ensure against unusual circumstances such as catastrophic events.
That non-admitted carriers operate outside of state insurance laws is not red flag signaling financial instability. State licensing, filing and reporting requirements are simply different for non-admitted carriers. Further, larger non-admitted carriers are usually well-capitalized subsidiaries of major financial services companies.
Due diligence however, demands that you check A.M. Best to determine the financial stability of any insurance company you're considering as your carrier.
Wholesale insurance agents place business brought to them by retail agents. Unlike a retail broker, wholesale brokers have a direct working relationship with the insurer, whereas the retail agent who produced the business does not. The same broker can function as a retailer or wholesaler, depending on the specific situation.
There are two types of wholesale brokers: managing general agents and surplus lines brokers. The latter work with retail agents and insurers to obtain coverage for the insured. Unlike a managing general agent, a surplus lines broker does not have binding authority from the insurer.
[Table of Content](#0.1)
___
## 28.) Actuarial Analyst Common Interview Questions
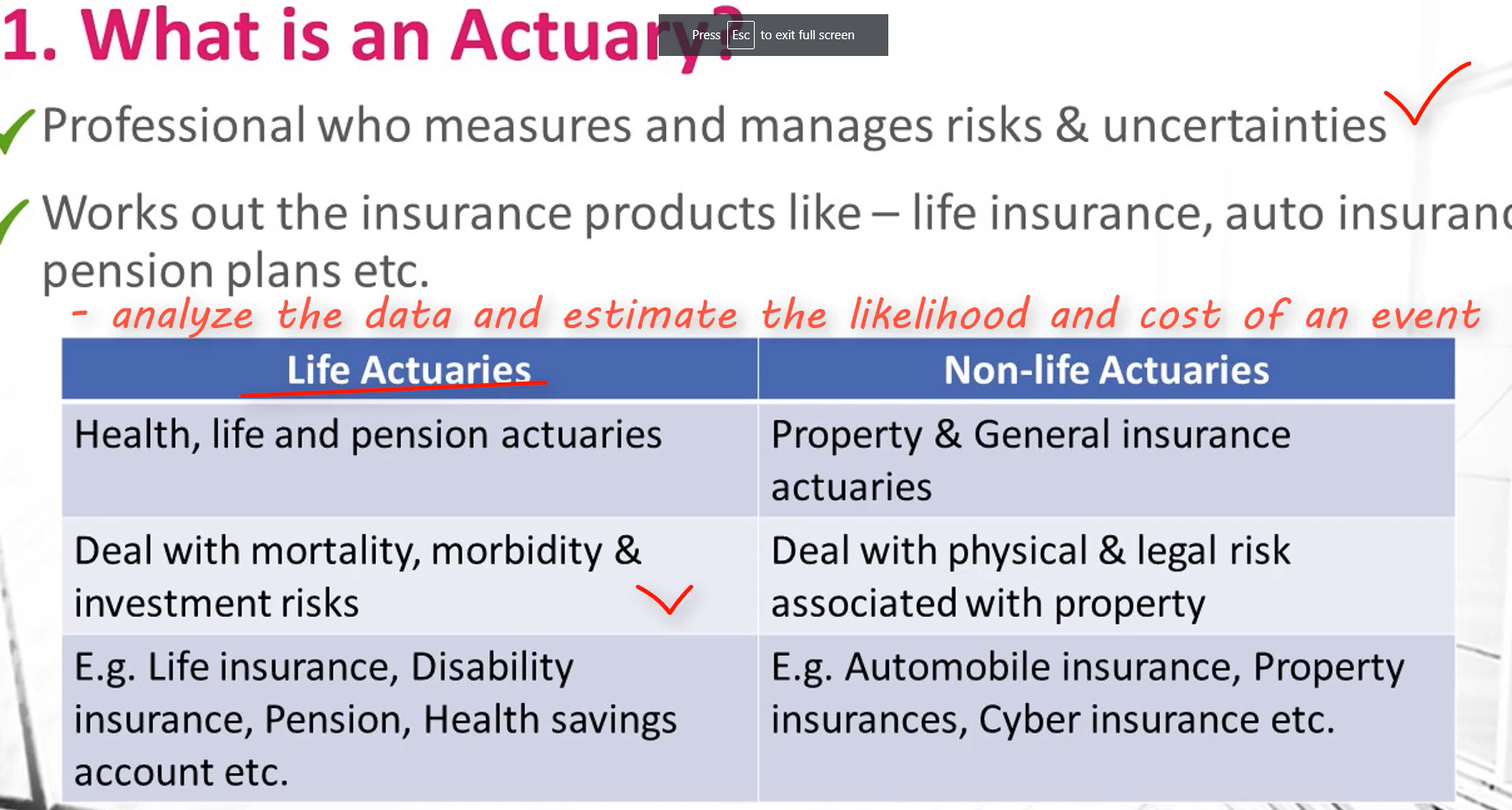



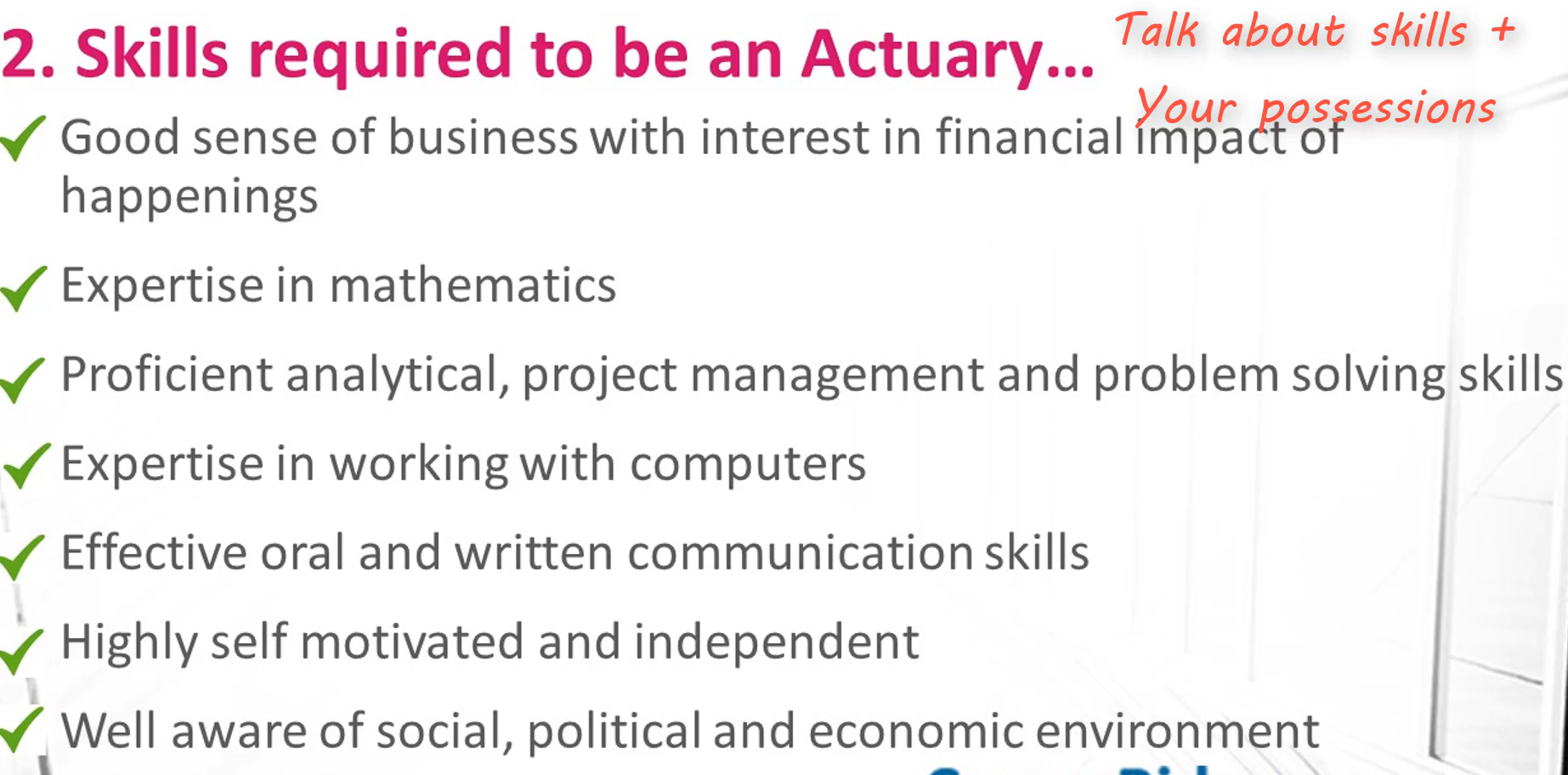
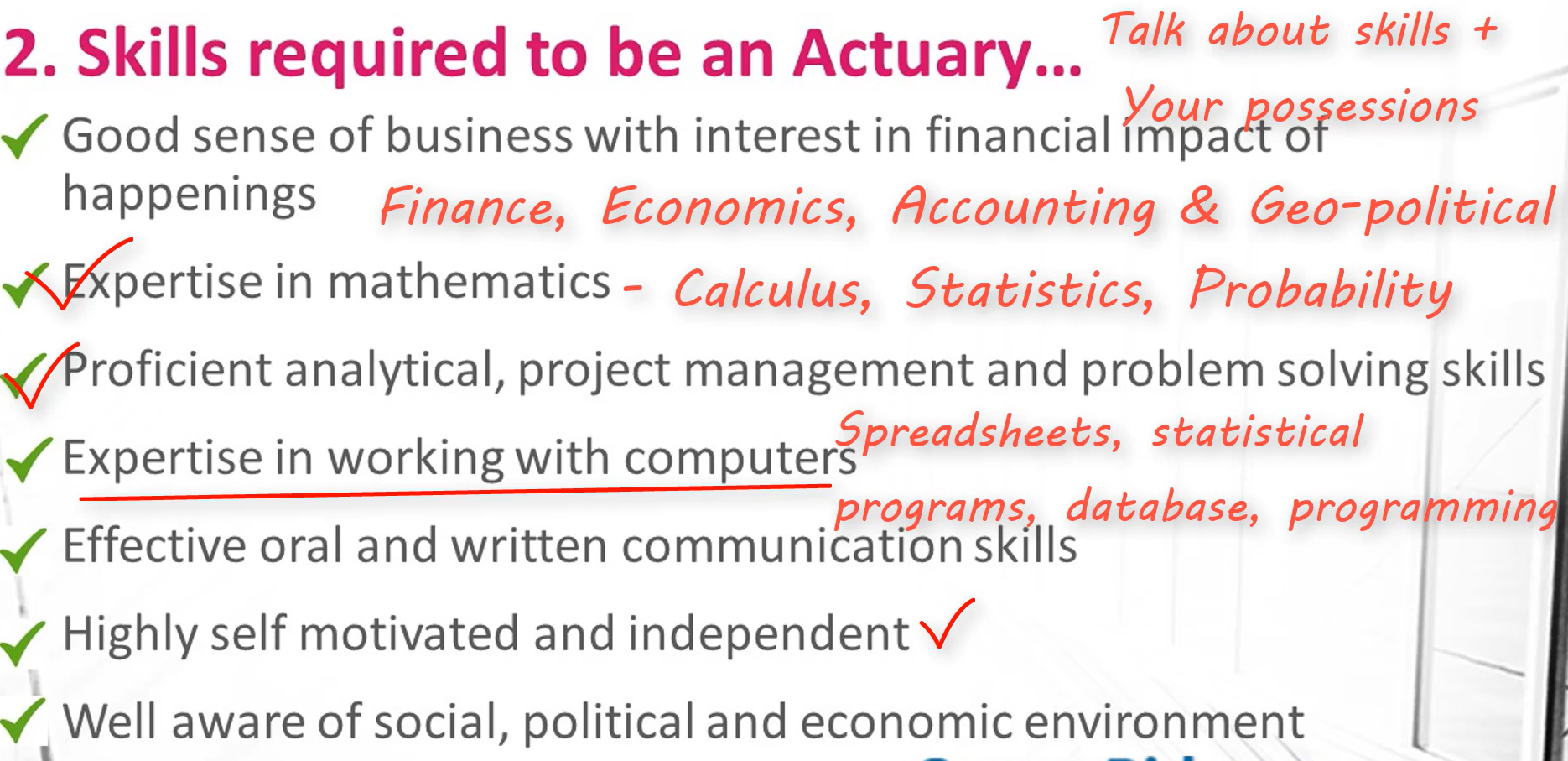

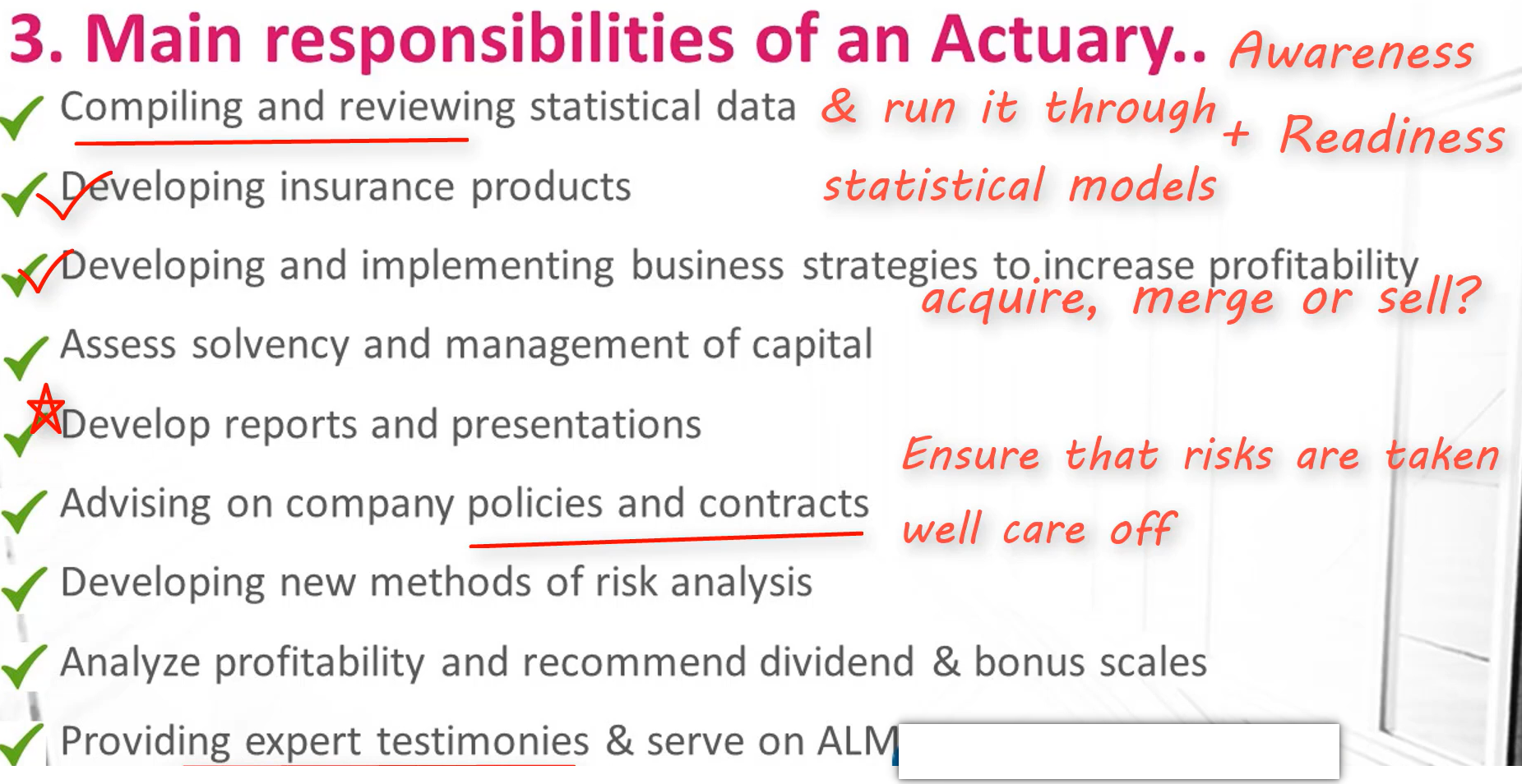






















___
## Author
[Table of Content](#0.1)
**
♡ Thank you for taking the time ♡**